All published articles of this journal are available on ScienceDirect.
The Efficacy of Bedside Chest Ultrasound in the Detection of Traumatic Pneumothorax
Abstract
Background
Chest X-rays have long been used to diagnose pneumothorax. In trauma patients, chest ultrasonography combined with chest CT may be a safer, faster, and more accurate approach. This could lead to better and quicker management of traumatic pneumothorax, as well as enhanced patient safety and clinical results.
Aim
The purpose of this study was to assess the efficacy and utility of bedside US chest in identifying traumatic pneumothorax and also its capacity to estimate the extent of the lesion in comparison to the gold standard modality chest computed tomography.
Methods
This was an observational cross-sectional study of 160 patients with traumatic pneumothorax. This sample was collected from all chest trauma patients admitted to Al-Kindy Teaching Hospital in Baghdad-Iraq between November 2021 and September 2022. Such patients were to have a bedside chest US and chest CT scan performed by a skilled radiologist to detect lung point signs and lung sliding, which would be used to determine the patient's pneumothorax status.
Results
According to the study's findings, about 77.5% of the patients evaluated were men. Furthermore, 40.6% of patients experienced blunt trauma. Chest ultrasound revealed positive pneumothorax in 50 cases (31.2%), while positive pneumothorax was confirmed by computed tomography in 53 cases (33.1%) with no significance in the detection of pneumothorax between the two imaging modalities p-value(0.719). Comparably, there was no significant difference in estimating the size of a pneumothorax between the two modalities (p-value = 0.547). Chest ultrasound diagnostic accuracy showed a sensitivity of approximately 92.45%, specificity of 99.07%, and diagnostic accuracy of 96.88%.
Conclusion
Our findings indicated that chest ultrasound might be a valuable rapid diagnostic tool for traumatic pneumothorax in the emergency department in addition to diagnosis. It eliminates the need to transport patients for a CT chest scan.
1. INTRODUCTION
Chest ultrasonography (US) is gaining popularity in the literature of critical care and emergency medicine. Recently, the US has been utilised to evaluate pneumothorax and other lung diseases. There is increasing interest in this beneficial technique as an alternative chest X-ray [1]. Plain chest radiographs are typically taken in patients with thoracic trauma to look for pneumothorax. However, radiographs in severely injured patients are taken in the supine position (AP—anteroposterior view), making it more difficult to see the typical pneumothorax features due to underlying spinal and other injuries [2, 3]. According to published research, radiographs taken at the time of the patient's initial presentation may not reveal a mild pneumothorax in up to 50% of trauma patients [4]. In the detection and evaluation of traumatic pneumothorax, bedside chest ultrasonography is a highly sensitive and specific tool, particularly in unstable patients. Furthermore, CT chest is regarded as the gold standard diagnostic technique for this condition. So, from the standpoint of biomedical engineering, chest ultrasound, and chest CT scan have produced a unique scenario in medicine: engineers are beginning to switch back to older technologies, favouring more efficient use of lung ultrasound in the severely ill [5].
2. NOVELTY OF THIS STUDY
This study introduced a significant advancement in the field of pneumothorax diagnosis by comprehensively evaluating the efficacy of chest ultrasound as a primary diagnostic tool. Unlike traditional methods that often involve radiation exposure, lack real-time capabilities, or require more invasive procedures, chest ultrasound offers a non-invasive, radiation-free approach that enables immediate visualization of the pleural space.
The novelty of our research lies in bridging existing gaps in current diagnostic practices. By systematically assessing the accuracy and reliability of chest ultrasound in detecting pneumothorax, this study aims to establish ultrasound as a frontline modality for initial diagnosis in clinical settings of pneumothorax and highlight its potential to improve patient outcomes through early and accurate detection.
3. LITERATURE REVIEW
The presence of air in the pleural space is known as pneumothorax (PTX), which can be spontaneous or nonspontaneous (traumatic). Traumatic PTX is a common life-threatening condition seen in the emergency room (ED). A traumatic pneumothorax can be caused by a blunt or penetrating injury, a rib fracture, diving, or flying [6]. Up to 50% of severe polytrauma patients with chest injuries have pneumothorax [7]. Pneumothorax can also be divided into three types: simple, tension, and open. A tension pneumothorax causes mediastinal structures to shift, whereas a simple pneumothorax does not. An open pneumothorax is a hole in the chest wall that allows air to enter and exit the body. [2]
Chest X-ray (CXR), computed tomography (CT), and thoracic ultrasound (US) are key modalities utilized for this purpose. CXR has traditionally been the initial imaging tool due to its widespread availability and ability to detect large pneumothoraces with reasonable sensitivity [2]. However, its sensitivity diminishes in cases of subtle or small pneumothoraces [8]. CT offers superior sensitivity and specificity compared to CXR, particularly in identifying small pneumothoraces and associated injuries, making it the gold standard for comprehensive evaluation in trauma settings [9]. In recent years, thoracic ultrasound has emerged as a valuable bedside tool for pneumothorax detection, offering advantages such as real-time imaging and the absence of radiation exposure [10]. Studies comparing these modalities have highlighted the complementary roles of CXR, CT, and US in the diagnosis and the management of traumatic pneumothorax, emphasizing the importance of tailored imaging appro- aches based on clinical presentation and resource availability [11]
Although chest CT is the gold standard in chest imaging, it is costly and cannot be performed on a regular basis. Furthermore, transferring critically ill patients to the radiology department entails considerable danger when paired with radiation exposure [12]. Additionally, thoracic ultrasound (US) has gained prominence in recent years for its diagnostic capabilities. Soldati et al. (2008) evaluated the diagnostic accuracy of lung ultrasonography in detecting occult traumatic pneumothorax, underscoring its potential as a frontline diagnostic tool in the emergency department. [13] It. is a highly sensitive and specific approach to the diagnosis and evaluation of a wide range of chest illnesses that eliminates the risk of transferring unstable patients as well as radiation exposure and is widely available in resource-constrained situations [14].
The goal of US scanning the chest was to examine one or more sonographic signals that corroborate or rule out PTX, such as lung sliding, lung pulses, and comet tails. The essential symptoms to look for in order to diagnose or rule out PTX are the lung sliding sign and the lung point sign. The indication for lung sliding is completely specific to PTX [15]. Therefore, in comparison to the gold standard study chest CT scan, the current study assesses the effectiveness and accuracy of bedside chest ultra- sonography in diagnosing traumatic PTX and estimates its size.
4. METHODS
4.1. Study Design and Setting
The participants in this observational cross-sectional study had a traumatic pneumothorax and were admitted to Al-Kindy Teaching Hospital in Baghdad, Iraq. The study was authorised by the ethics committee with reference number 1148, and all subjects signed informed consent (Oral consent was taken from women who desired to participate in this research). This study took place between November 2021 and September 2022.
4.2. Sample Size and Bias
The study was based on a convincing sample of 160 cases of traumatic PTX. To address potential sources of bias in the study, several measures were implemented. Firstly, rigorous inclusion criteria were established to ensure the homogeneity of the study population, limiting the potential for selection bias. Additionally, efforts were made to standardize the diagnostic criteria for pneumothorax assessment across all study participants, minimizing measurement bias. Furthermore, the study employed a blinded assessment of chest ultrasound findings by experienced radiologists to reduce observer bias.
The study size was determined through a comprehensive review of the existing literature on chest ultrasound in pneumothorax diagnosis. Based on prior studies and meta-analyses, a sample size calculation was performed to ensure adequate statistical power and sufficient statistical power to detect a predetermined effect size with a specified level of confidence (95%).
These patients were included and excluded from this investigation based on the following criteria:
4.3. Inclusion Criteria
1. Patients of any age or gender who have experienced blunt or penetrating chest trauma.
2. Patients who had a chest ultrasound for trauma followed by a chest CT.
4.4. Exclusion Criteria
1. Patients who do not have a CT chest because they are not stable enough to go.
2. Patients suffering from a potentially fatal condition (tension pneumothorax).
3. Patients with limited imaging acquisition have surgical injuries and chest dressings that can change or prevent ultrasound beam transmission to the lung.
4.5. Data Collection Procedure
Patients were enrolled in the research study after performing a chest CT scan. Before the CT scan, a bedside chest ultrasound was performed. During the initial evaluation of patients satisfying trauma criteria, the radiologist performed a bedside US examination of the chest.
During the first evaluation of trauma patients, the radiologist performed bedside US evaluations of the chest with (GE Voluson E6 ultrasound machine)using a superficial probe (11L-D) at a frequency of 3-11 MHz. Patients undergo scanning while positioned in a supine or near-supine posture. The ultrasound probe is appro- priately positioned sagittally, with its indicator directed cephalad, over the anterior chest wall, specifically targeting the second intercostal space along the mid-clavicular line. The sonographer's initial task involves identifying two ribs with posterior shadowing, thereby revealing the pleural line located between them. This characteristic presentation, colloquially termed 'the bat sign,' illustrates the resemblance to bats, with the ribs' periosteum representing the wings and the bright hyperechoic pleural line depicting the bats' body. In instances where rib visualization is lacking, the probe should be gradually maneuvered in a caudal (inferior) direction until two ribs become discernible on the screen. The region between these identified rib landmarks facilitates the observation of the parietal and visceral layers of the pleura as they exhibit sliding motion relative to each other [16]. The views included four locations of each pneumothorax (anterior second intercostal space at the midclavicular line, fourth intercostal space at the anterior axillary line, sixth intercostal space at the midaxillary line, and sixth intercostal space at the posterior axillary line) each examined by two modes,the brightness (B-mode) looking for the presence of plural sliding in each region (like the shimmering of the pleural or the sign of an ant on a log). If the lung point sign (transition from sliding to non-sliding pleura) was observed in any of these views, or if the sliding lung sign was absent, consider a positive pneumothorax by chest US. An additional indication by the B mode known as “Comet-tail artifacts” appears as continuous hyperechoic vertical lines that run from the pleura to the edge of the screen, moving in unison with respiratory activity and lung sliding. In patients with pneumothorax, ultrasound imaging revealed the absence of 'comet-tail artifacts.' This absence is attributable to air accumulation within the pleural cavity, impeding sound wave propagation and disrupting the acoustic impedance gradient. Furthermore, since 'comet-tail' artifacts originate from the visceral pleura, which becomes non-visible in pneumothorax, these artifacts are not generated under such circumstances, and by the motion (M-mode) looking for the normal sliding of the pleura giving sea shore sign or abnormal un sliding pleura which indicate underlying pneumothorax which will give barcode sign. Regarding the quantification of the plural air volume in a positive patient, positive pneu- mothorax found in the 1st and 2nd views is considered minimal; positive pneumothorax reaching the 3rd view is considered mild; and if it reaches the 4th view, it is moderate in volume. A subsequent chest CT scan was performed on the patient with (SEIMENS 64 SLICE) in the supine position,image acquisition in the axial section 1 mm slice thickness with reconstruction into coronal and sagittal views interpreted by an experienced radiologist regarding the presence of pneumothorax by evaluation with lung window, window width (WW) ranges from about 1500 to 2000 Hounsfield Units (HU), and the window level (WL) is set between -500 to -700 HU, and quantify its amount as (minimal <25%, mild 25-50% and moderate >50%) according to the protocol performed by Collins et al. [17]. The determination of pneumothorax volume percentage involved the manual delineation of regions of interest encompassing the periphery of the collapsed lung and the inner boundary of the ipsilateral hemithorax across each sectional image.The findings of the two tests were documented and compared in order to assess the chest US's accuracy in identifying traumatic PTX in comparison to the gold standard modality, CT chest. The hospital research committees at Alkindy Teaching Hospital gave their approval based on ethical considerations.
4.6. Statistical Analysis
To statistically analyze the data, the Statistical Package for Social Sciences 20 for Windows was utilised. The 95% confidence interval was employed. For quantitative data, a normal distribution, indicated by the mean SD, will be present. The data categories, along with frequency and percentages, will be displayed. The following metrics were used to analyse the performance of thoracic sonography and CT chest: sensitivity, specificity, positive and negative predictive values, and likelihood ratios. Regarding missing data employing a combination of preventive measures, imputation techniques, sensitivity analyses, and subgroup analyses, the study aimed to minimize the impact of missing data on the validity and reliability of the study findings while ensuring transparency and rigor in data handling and analysis.
| Demographic data | No. | % |
|---|---|---|
|
Age (years) < 35 ≥35 |
110 50 |
68.7 31.3 |
| Mean±SD | 31.75 ± 9.17 | |
| Range | 17-60 | |
| Median | 32 | |
|
Gender Male Female |
124 36 |
77.5 22.5 |
| Variables | No. | % |
|---|---|---|
|
Mode of trauma Blunt trauma Penetrating trauma |
65 95 |
40.6 59.4 |
|
Site of trauma Right side Left side Bilateral |
62 53 45 |
38.8 33.1 28.1 |
| - | Pneumothorax Diagnosis by Ultrasound | Pneumothorax Diagnosis by Computed Tomography | Chi–square Test | |||
|---|---|---|---|---|---|---|
| - | n | % | n | % | X2 | P |
| Negative | 110 | 68.8 | 107 | 66.9 | - | - |
| Positive | 50 | 31.2 | 53 | 33.1 | 0.129 | 0.719 |
The data supporting the findings of the article is available in the [zenodo repository] at [https://zenodo .org/uploads/12685922], with DOI 10.5281/zenodo.126 85921.
5. RESULTS
One hundred sixty patients participated in the study, 36 were females (22.5%), and 124 were males (77.5%). The patients' ages (years) ranged from 17 to 60, with a mean±SD of 31.75 ± 9.17, (Table 1).
Penetrating trauma was the most common type of trauma (59.4%) while blunt trauma represented (40.6%). The right side of the chest was affected in 62 cases (38.8%), the left side in 53(33.1%), and there was bilateral affection in 45 cases (28.1%), (Table 2).
As regards the statistical significance in the diagnosis of pneumothorax between CT and chest US in the detection of traumatic PTX results, chest US showed positive PTX in 50 cases (31.2%). Among them, 53 cases (33.1%) were proved to be positive by CT. While 110 cases were negative by US (68.8%) and 107 (66.9%) were negative by CT (Table 3). The comparison between chest ultrasound (U.S.) and chest CT scan indicates that there is no statistically significant difference in their ability to detect pneumothorax with p p-value of 0.719.
Regarding the diagnostic efficacy of chest ultrasound (US) in detecting pneumothorax, the study reported an overall accuracy of 96.8%. The sensitivity was found to be 92.4%, indicating the proportion of true positive cases correctly identified. Specificity was notably high at 99.0%, reflecting the accuracy in identifying true negative cases. Additionally, the positive predictive value was 98.0%, indicating the likelihood of a positive test result accurately predicting the presence of pneumothorax, while the negative predictive value was 96.3%, highlighting the accuracy in ruling out pneumothorax when the test result is negative (Table 4).
Regarding the size of pneumothorax evaluated by chest ultrasound and chest CT scan, Lesion of PTX was minimal (22.4%) when diagnosed by chest US compared to (32.1%) when diagnosed by chest CT. On the other hand, lesions of PTX were mild (57.1%) when diagnosed by chest
| - | Value | 95% CI |
|---|---|---|
| Sensitivity | 92.45% | 81.8 – 97.9 |
| Specificity | 99.07% | 94.9 – 99.9 |
| Positive predictive value | 98.00% | 89.4 – 99.9 |
| Negative predictive value | 96.36% | 90.9 – 99.0 |
| Accuracy | 96.88% | 92.9 – 98.9 |
| - | Chest Ultrasound (n=49) | Chest Computed Tomography (n=53) | Chi – Square Test | |||
|---|---|---|---|---|---|---|
| - | n | % | n | % | X2 | P |
| Minimal | 11 | 22.4 | 17 | 32.1 | - | - |
| Mild | 28 | 57.1 | 26 | 49.1 | - | - |
| Moderate | 10 | 20.4 | 10 | 18.9 | 1.205 | 0.547 |
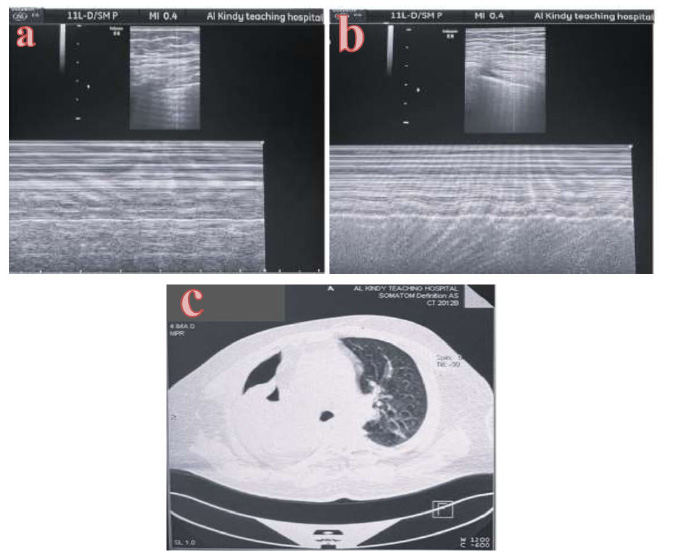
Diagnosis of mild right-sided pneumothorax by bedside chest ultrasonography and CT scan.
32 years old male presented with chest trauma diagnosed with moderate right-sided pneumo- thorax: (a): bedside chest ultrasound,(M mode) shows the barcode sign at the sixth intercostal space, anterior axillary line of the right hemithorax(indicate pneumothorax) (b): bed side chest ultrasound,(M mode) shows the normal sea shore sign at the second intercostal space,mid clavicular line of the left hemithorax (normal pleural) (c): CT scan of the chest for the same patient axial view (lung window) shows moderate right-sided pneumothorax.
US compared to (49.1%) when diagnosed by chest CT. Also, the Lesion of PTX was moderate (20.4%) when diagnosed by chest US compared to (18.9%) when diagnosed by chest CT. with no statistical significance between the two studies regarding the estimation of the volume of pneumothorax,(p value 0.547) (Table 5).
6. DISCUSSION
Traumatic pneumothorax is a dangerous condition that requires immediate medical attention. Chest X-rays are commonly used to diagnose it; however, they may not detect the existence of a mild pneumothorax, particularly in the supine position. Lung ultrasonography is showing promise in diagnosing pneumothorax in trauma patients. In addition to having various intrinsic benefits over chest radiography, lung ultrasonography is more sensitive in diagnosing traumatic pneumothorax than supine chest X-rays. To rule out pneumothorax, it should be included in the immediate examination of thoracic trauma patients [ 18 ].
A total of 160 patients with chest trauma were included in this large-scale prospective clinical research, assessing the utility of bedside chest US and chest CT in diagnosing traumatic pneumothorax. Blaivas et al. conducted a similar study involving 176 adult blunt trauma patients, employing a 2-point 4 MHz micro-convex probe for chest US in the emergency department setting [ 19 ]. Penetrating trauma was predominant in our study (59.4%), followed by blunt trauma (40.6%). Thoracic trauma remains a significant concern, affecting approximately 60% of polytrauma patients with a mortality rate ranging from 20% to 25% [ 20 ].
Regarding the comparison between chest US and chest CT in detecting traumatic PTx, chest US identified positive PTx in 50 cases (31.2%), with 53 cases (33.1%) confirmed by chest CT. Negative findings were reported in 110 cases (68.8%) by chest US and 107 cases (66.9%) by chest CT, indicating no statistically significant difference in diagnostic outcomes between the two modalities. This finding is consistent with Vafaei et al., who reported similar results in 152 chest trauma patients, highlighting the complementary roles of different imaging techniques in trauma assessment [ 21 ].
Our study demonstrated high diagnostic accuracy for both chest US and chest CT in diagnosing traumatic pneumothorax, with an overall accuracy of 96.8%. Specifically, chest US showed a sensitivity of 92.4%, specificity of 99.0%, positive predictive value of 98.0%, and negative predictive value of 96.3%. These results align closely with findings by Ianniello et al., who conducted a retrospective study on blunt trauma patients using a 7.5 MHz scanner [ 22 ].
Nagarsheth and Kurek's prospective study also compared thoracic ultrasound with CXR and CT scan in diagnosing traumatic pneumothorax, highlighting ultrasound's superior sensitivity (81.8%) compared to CXR (31.8%) and comparable specificity (100%) with CT [ 23 ]. Our study's specificity (100%) stands out as the highest reported, reflecting the reliability of chest US in ruling out false positives.
.Quantitative comparisons of PTx size using the Spearman correlation coefficient between chest US and CT further validate its reliability in clinical practice, consistent with findings by Abu Arab et al. [ 24 ]. Future research should focus on validating these findings in larger cohorts to establish standardized protocols for trauma imaging assessment.
CONCLUSION
Chest ultrasound emerges as a promising and practical diagnostic tool for pneumothorax, offering distinct advantages over conventional imaging modalities such as chest X-ray (CXR) and computed tomography (CT). Its real-time imaging capability, portability, and avoidance of ionizing radiation make thoracic ultrasound (US) well-suited for prompt and precise diagnosis, particularly in urgent clinical settings like trauma centers and emergency departments. The integration of thoracic ultrasound into clinical workflows facilitates bedside evaluation, enabling immediate decision-making and reducing the need for patient transfer to radiology suites. Beyond initial diagnosis, ultrasound's ability to monitor pneumothorax dynamics and guide interventions underscores its pivotal role in enhancing patient care and outcomes. Future advancements in ultrasound technology hold promise for further improving diagnostic accuracy and expanding its application in diverse healthcare settings.
LIMITATIONS OF THE STUDY
The inclusion of all ages and injuries to the thorax, including those caused by penetrating and blunt trauma, may be considered a limitations of this study.
AUTHORS’ CONTRIBUTIONS
Saja Ali Ahmed performed all chest ultrasound scanning and contributed extensively to the interpretation of the data and the conclusion. Shaymaa Khalid Abdul-Qader performed all the chest CT scan procedures for participating patients, as well as data gathering, statistical data analysis, and interpretation of data. Nabaa Aswad Shakir provided the first draft of the manuscript before its publication, and participated in all the research steps. All authors revised and approved the final manuscript.
LIST OF ABBREVIATIONS
| PTX | = Pneumothorax |
| US | = Ultrasound |
| CXR | = Chest X-ray |
| CT | = Computed Tomography |
| ED | = Emergency Department |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was authorised by the ethics committee of Al-Kindy Teaching Hospital in Baghdad, Iraq, with reference number 1148.
HUMAN AND ANIMAL RIGHTS
All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, as well as the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
CONSENT FOR PUBLICATION
All subjects signed informed consent (Oral consent was taken from women who desired to participate in this research).


