All published articles of this journal are available on ScienceDirect.
Attention Deficit Hyperactivity Disorder Symptoms Among Students Attending Higher Educational Institution: A Cross-Sectional Study
Abstract
Background
A complicated and clinically varied illness known as ADHD (“Attention-deficit/hyperactivity disorder”) leads to poor academic and professional outcomes, family stress, and financial difficulty. Worldwide, children and adults with attention-deficit/hyperactivity disorder are likely to suffer from all problems. ADHD are neurodevelopmental diseases that impact impulsivity, hyperactivity, and inattention. Basic academic skills like reading and arithmetic have been connected to visual search and sustained visual attention.
Methodology
The prevalence of attention-deficit/hyperactivity symptoms among students aged 17 to 23 in higher education institutions in Punjab, India, was investigated through a cross-sectional quantitative survey conducted from May to September 2023.. An online form was used to create the ADHD self-report scale (v1.1). This questionnaire was divided into 3-part inattention, hyperactivity, and impulsivity. The responses were categorized into five levels: Never, Rarely, Sometimes, Often, and Very Often. This Questionnaire was distributed to students from higher educational institutes, and data was collected.
Result
The total 360 student data were analyzed using SPSS 20. As the age increased, ADHD symptoms were reduced, inattention was most symptomatic in 18 and 19 years,` and hyperactivity and impulsivity symptoms had high scores in the 23 years age category. Out of the participants, 228 were female and 132 were male. Female students exhibited more symptoms of inattention (37.7%), while male students showed higher symptoms of hyperactivity (39.4%) and impulsivity (31.8%). Most students reported experiencing symptoms 'sometimes,' with responses indicating 'often' or 'very often' being rare across all three categories. This suggests that many respondents experience ADHD-related symptoms. Factors such as the number of siblings, family type, parents’ education level, and living arrangements did not impact the prevalence of ADHD symptoms.
Conclusion
The prevalence rate of ADHD symptoms among north Indian higher educational institutes was 23.3%. Among these ADHD-symptomatic students, inattention was 35%, hyperactivity 39.2%, and Impulsivity 26.9%, respectively.
1. INTRODUCTION
ADHD (“Attention-Deficit/Hyperactivity Disorder”) is a complex neurodevelopmental/neurological, mental comorbidity, psychosocial, and clinically variable syndrome that impacts demographic, psychosocial, psychiatric, and cognitive abnormalities that lead to financial hardship, family stress, and poor scholastic and career results. Worldwide, children with attention-deficit/hyperactivity disorder are highly likely to suffer from these problems that persist till adult age, and adults with ADHD have shown similar clinical characteristics along with mood or anxiety problems as well as conduct or oppositional defiant disorders [1-3]. In the past, the term ADD (“attention deficit disorder”) was used to characterize the subtype of ADHD in which inattention, rather than hyperactivity, was the main symptom. Currently, ADHD is diagnosed based on the diagnostic and statistical Manual of Mental Disorders 5 (DSM-5) criteria and shows 3 different types of symptoms: inattentive, hyperactive/impulsive, and a combination of both [4]. A child must have shown six or more signs of impulsivity, hyperactivity, or inattention for at least six months before turning twelve to be diagnosed with ADHD. Both the hyperactive/impulsive and inattentive subtypes of ADHD are included, and a diagnosis of ADHD necessitates the fulfillment of particular requirements [5-8]. ADHD diagnostic symptoms are considered as Attention-Deficit/Hyperactivity Symptoms (ADHS). These diagnostic symptoms are also called ADHD symptoms [9]. The neurological disorder can also be diagnosed with the help of Magnetic Resonance Imaging (MRI), neural trans- mitters, smartphone based Convolutional Neural Networks (CNN) or Natural Language Processing (NLP) and Electroencephalography (EEG), including ADHD [10-12]. Research on the history of ADHD in families has repeatedly demonstrated a significant familial component and hereditary factors. According to structural and functional imaging studies, the etiology of ADHD includes anomalies in the dopaminergic and noradrenergic systems as well as malfunctions in the fronto-subcortical pathways [13-15]. ADD or ADHD mainly impacts attention, and “psychology defines attention as the process through which one chooses and focuses on certain environmental stimuli. Attention has a limited capacity for receiving stimuli. The number of things or objects a person can concentrate on during a brief exposure is known as the attention span [3, 4]. Three facets of human attention are investigated: processing speed, selectivity, and awareness. These components may be experimentally isolated, and their interactions can be investigated in the context of comparable tasks [16-18]. A stimulus was shown to enhance stimulus selection, raise awareness for processing all external information, or do both simultaneously. Despite the fact that the development of awareness and selectivity are separate processes, they may coexist without interference [18]. Visual span refers to the number of letters or characters that a person can identify accurately in one fixation without moving their eyes. It is considered an important measure of reading ability, as it reflects how efficiently the brain processes visual information during reading. The larger the visual span, the faster and more accurate the reading performance [19]. Visual search and sustained visual attention have been linked to fundamental academic abilities, including reading and numeracy. Visual search refers to the encoding and categorizing procedure [20-22]. Visual attention span refers to the amount of visual information that a person can process and remember at a single glance. It is an important component of reading comprehension because it affects a reader's ability to perceive and integrate information from the text [23].
2. METHODOLOGY
A cross-sectional quantitative study was carried out from May to September 2023 to determine the prevalence of attention-deficit/hyperactivity symptoms among students of higher educational institutes aged from 17 to 23 years. A convenience sampling technique was used to collect the samples, and the sample size was calculated based on the study design.
Sample Size= Z1-α/22p(1-p) / d2
Z-statistic (Z): Z value is 1.96 at 5% type 1 error and 95% confidence intervals in this investigation. The proportion (prevalence) that was obtained from earlier research is known as the expected proportion (P). In India, the prevalence of adult ADHD was 36% [24, 25]. Thus, p equals 0.36. Precision (d): Investigators must have a thorough understanding of this value. It is possible to infer from the formula that the sample size varies inversely with the precision squared (d2) [26, 27]. Instead of being a percentage, d in the calculation should be a proportion of one, and the average number of samples that Cohon D suggested d was 0.5 [28].
n = 1.962 * 0.36(1- 0.36) / 0.052
= 3.84*0.36*0.64 / 0.0025
=3.84*0.2304/0.0025
= 0.8852/0.0025
= 354
A total of 360 students from higher educational institutes in Punjab were considered for this study, considering that few of them could leave the questionnaires half-filed or wrongly filled out. Students with the best corrected (glasses, contact lenses) visual acuity of 20/20 at a distance and N6 at near were included in this study, and students with a history of any ocular injury, surgery, infection in the eye, currently taking any medication, diagnosed ADHD patients or any learning or mental disorder, head trauma, received or receiving any kind of psychological, behavioural, occupational, and vision therapy, and general health issues were excluded. The research protocol was presented to the university ethical committee, and ethical approval was obtained for conducting this study from the Punjab Ethical Committee at Chitkara University, Punjab, India. An ethical clearance certificate was obtained with ethical registration no. IHEC/CU/PB/DHR/23/182. 18 ADHD questionnaires (ADHD self-report scale v1.1) [29-32] were constructed in Google form along with basic history, as mentioned in Table 6. First, approval was obtained from the higher educational institute (HEI) after the questionnaire was circulated electronically in each HEI classroom, and the students were asked to participate. Informed consent was obtained from whoever wanted to participate, ensuring that their information would be kept secret and used for research work only. When student participation reached a 360 number, data collection was stopped and analyzed using Excel and SPSS 20 crosstab, and a person correlation test was performed along with a graph.
3. RESULTS
The age range was 17 to 23 years, with a mean of 18.95 + 1.13 years. Out of 360 students, 228 were female, and 132 were male, which was 63.3% and 36.7% respectively. This questionnaire likely assesses various aspects related to inattention, hyperactivity, and impulsivity. The responses were categorized into five levels: never, rarely, sometimes, often, and very often.
Table 1 shows the number of responses from each category of question: inattention (AT), hyperactivity (HA), and impulsivity (IM), and the maximum responses were from rarely and sometimes. Very few responses were from very often in all 3 categories. Overall, “Sometimes” was the highest count across all three categories, which indicates that many respondents experience these ADHD-related symptoms occasionally and exhibit ADHD-related issues. “Very Often” has consistently low counts in all three categories, suggesting that few respondents reported experiencing symptoms at a very high frequency. “Sometimes” might be considered a moderate level of symptom frequency, while “Very Often” represents a high frequency. 126 students had moderate symptoms of inattention, 141 students had hyperactive symptoms, and 97 students had impulsivity symptoms.
| - | AT1 | AT2 | AT3 | AT4 | AT5 | AT6 | HA1 | HA2 | HA3 | HA4 | HA5 | HA6 | IM1 | IM2 | IM3 | IM4 | IM5 | IM6 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Never | 55 | 53 | 87 | 64 | 48 | 56 | 36 | 36 | 94 | 54 | 31 | 157 | 32 | 73 | 71 | 64 | 68 | 151 |
| Rarely | 118 | 113 | 110 | 96 | 78 | 86 | 114 | 59 | 122 | 115 | 69 | 96 | 82 | 122 | 110 | 122 | 106 | 114 |
| Sometimes | 139 | 149 | 114 | 142 | 132 | 146 | 142 | 141 | 102 | 98 | 127 | 73 | 151 | 107 | 112 | 117 | 127 | 70 |
| Often | 37 | 33 | 38 | 42 | 65 | 55 | 46 | 86 | 26 | 62 | 82 | 24 | 62 | 40 | 45 | 45 | 40 | 15 |
| Very Often | 11 | 12 | 11 | 16 | 37 | 17 | 22 | 38 | 16 | 31 | 51 | 10 | 33 | 18 | 22 | 12 | 19 | 10 |
| Total | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 | 360 |
| - | Inattention | Hyperactivity | Impulsivity | ADHD | ||||
|---|---|---|---|---|---|---|---|---|
| - | Frequency | Percent | Frequency | Percent | Frequency | Percent | Frequency | Percent |
| NS | 234 | 65.0 | 219 | 60.8 | 263 | 73.1 | 276 | 76.7 |
| SYM | 126 | 35.0 | 141 | 39.2 | 97 | 26.9 | 84 | 23.3 |
| Total | 360 | 100.0 | 360 | 100.0 | 360 | 100.0 | 360 | 100.0 |
| - | Inattention | Hyperactivity | Impulsivity | ADHD | - | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| NS | SYM | NS | SYM | NS | SYM | NS | SYM | - | ||
| Female | Count | 142 | 86 | 139 | 89 | 173 | 55 | 176 | 52 | 228 |
| % within Gender | 62.30% | 37.70% | 61.00% | 39.00% | 75.90% | 24.10% | 77.20% | 22.80% | 100.00% | |
| % within category | 60.70% | 68.30% | 63.50% | 63.10% | 65.80% | 56.70% | 63.80% | 61.90% | 63.30% | |
| % of Total | 39.40% | 23.90% | 38.60% | 24.70% | 48.10% | 15.30% | 48.90% | 14.40% | 63.30% | |
| Male | Count | 92 | 40 | 80 | 52 | 90 | 42 | 100 | 32 | 132 |
| % within Gender | 69.70% | 30.30% | 60.60% | 39.40% | 68.20% | 31.80% | 75.80% | 24.20% | 100.00% | |
| % within category | 39.30% | 31.70% | 36.50% | 36.90% | 34.20% | 43.30% | 36.20% | 38.10% | 36.70% | |
| % of Total | 25.60% | 11.10% | 22.20% | 14.40% | 25.00% | 11.70% | 27.80% | 8.90% | 36.70% | |
| Total | Count | 234 | 126 | 219 | 141 | 263 | 97 | 276 | 84 | 360 |
| % of Total | 65.00% | 35.00% | 60.80% | 39.20% | 73.10% | 26.90% | 76.70% | 23.30% | 100.00% | |
Table 4.
| - | Inattention | Hyperactivity | Impulsivity | ADHD | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| NS | SYM | NS | SYM | NS | SYM | NS | SYM | |||
| 17 | Count | 15 | 7 | 14 | 8 | 15 | 7 | 16 | 6 | 22 |
| % within Age | 68.2% | 31.8% | 63.6% | 36.4% | 68.2% | 31.8% | 72.7% | 27.3% | 100% | |
| % within Category | 6.4% | 5.6% | 6.4% | 5.7% | 5.7% | 7.2% | 5.8% | 7.1% | 6.1% | |
| % of Total | 4.2% | 1.9% | 3.9% | 2.2% | 4.2% | 1.9% | 4.4% | 1.7% | 6.1% | |
| 18 | Count | 98 | 51 | 93 | 56 | 108 | 41 | 117 | 32 | 149 |
| % within Age | 65.8% | 34.2% | 62.4% | 37.6% | 72.5% | 27.5% | 78.5% | 21.5% | 100% | |
| % within Category | 41.9% | 40.5% | 42.5% | 39.7% | 41.1% | 42.3% | 42.4% | 38.1% | 41.4% | |
| % of Total | 27.2% | 14.2% | 25.8% | 15.6% | 30.0% | 11.4% | 32.5% | 8.9% | 41.4% | |
| 19 | Count | 66 | 38 | 59 | 45 | 76 | 28 | 76 | 28 | 104 |
| % within Age | 63.5% | 36.5% | 56.7% | 43.3% | 73.1% | 26.9% | 73.1% | 26.9% | 100% | |
| % within Category | 28.2% | 30.2% | 26.9% | 31.9% | 28.9% | 28.9% | 27.5% | 33.3% | 28.9% | |
| % of Total | 18.3% | 10.6% | 16.4% | 12.5% | 21.1% | 7.8% | 21.1% | 7.8% | 28.9% | |
| 20 | Count | 33 | 18 | 33 | 18 | 40 | 11 | 40 | 11 | 51 |
| % within Age | 64.7% | 35.3% | 64.7% | 35.3% | 78.4% | 21.6% | 78.4% | 21.6% | 100% | |
| % within Category | 14.1% | 14.3% | 15.1% | 12.8% | 15.2% | 11.3% | 14.5% | 13.1% | 14.2% | |
| % of Total | 9.2% | 5.0% | 9.2% | 5.0% | 11.1% | 3.1% | 11.1% | 3.1% | 14.2% | |
| 21 | Count | 10 | 8 | 11 | 7 | 14 | 4 | 14 | 4 | 18 |
| % within Age | 55.6% | 44.4% | 61.1% | 38.9% | 77.8% | 22.2% | 77.8% | 22.2% | 100% | |
| % within Category | 4.3% | 6.3% | 5.0% | 5.0% | 5.3% | 4.1% | 5.1% | 4.8% | 5.0% | |
| % of Total | 2.8% | 2.2% | 3.1% | 1.9% | 3.9% | 1.1% | 3.9% | 1.1% | 5.0% | |
| 22 | Count | 7 | 3 | 6 | 4 | 8 | 2 | 8 | 2 | 10 |
| % within Age | 70.0% | 30.0% | 60.0% | 40.0% | 80.0% | 20.0% | 80.0% | 20.0% | 100% | |
| % within Category | 3.0% | 2.4% | 2.7% | 2.8% | 3.0% | 2.1% | 2.9% | 2.4% | 2.8% | |
| % of Total | 1.9% | 0.8% | 1.7% | 1.1% | 2.2% | 0.6% | 2.2% | 0.6% | 2.8% | |
| 23 | Count | 5 | 1 | 3 | 3 | 2 | 4 | 5 | 1 | 6 |
| % within Age | 83.3% | 16.7% | 50.0% | 50.0% | 33.3% | 66.7% | 83.3% | 16.7% | 100% | |
| % within Category | 2.1% | 0.8% | 1.4% | 2.1% | 0.8% | 4.1% | 1.8% | 1.2% | 1.7% | |
| % of Total | 1.4% | 0.3% | 0.8% | 0.8% | 0.6% | 1.1% | 1.4% | 0.3% | 1.7% | |
| Total | Count | 234 | 126 | 219 | 141 | 263 | 97 | 276 | 84 | 360 |
| % within Age | 65.0% | 35.0% | 60.8% | 39.2% | 73.1% | 26.9% | 76.7% | 23.3% | 100% | |
Table 2 shows the count and percentages of inattention, hyperactivity, impulsivity, and overall ADHD within non-symptomatic and symptomatic students. 65%, 60.8%, 73.1%, and 76.7%, respectively, non-symptomatic students were there in higher educational institutes, and 35%, 39.2%, 26.9%, and 23.3%, respectively, symptomatic students were present among higher educational institutes. This table shows the highest percentage of symptomatic students were present in the hyperactivity category, then inattention, and the lowest category in impulsivity among the 23.3% ADHD symptomatic students.
Table 3 shows the prevalence of ADHD symptoms among male and female students, categorized by inattention, hyperactivity, impulsivity, and overall ADHD. Female students generally had a higher proportion of non-symptomatic cases compared to males across all categories. For inattention, 68.3% of females and 31.7% of males were symptomatic. For hyperactivity, 63.1% of females and 36.9% of males were symptomatic. For impulsivity, 56.7% of females and 43.3% of males were symptomatic. Overall, 61.9% of females and 38.1% of males were symptomatic for ADHD. This table also shows that within 35% of inattention, 23.9% female and 11.1% male, 39.2% of hyperactivities, 24.7% female and 14.4% male, 26.9% of impulsivity, 15.3% female and 11.7% male and 23.3% Overall ADHD, 14.4% female and 8.90% male was present.
Table 4 shows the prevalence of ADHD based on age; the age was distributed between 17 to 23 years, and prevalence was checked among students from higher educational institutes in inattention, hyperactivity, impulsivity, and overall ADHD, categorized by symptomatic (SYM) and Non-Symptomatic (NS) cases. For inattention, the percentage of symptomatic cases generally decreases with age, from 68.2% at age 17 to 55.6% at age 21, then slightly increases to 70% at age 22, and drops to 83.3% at age 23. For hyperactivity, the percentage of symptomatic cases fluctuates across age groups, with the highest at 64.7% for ages 20 and 21, and the lowest at 50% for age 23. For impulsivity, the percentage of symptomatic cases decreases with age, from 68.2% at age 17 to 33.3% at age 23. Overall, the pattern of ADHD symptoms mirrors that of inattention, with the percentage of symptomatic cases initially decreasing with age, from 72.7% at age 17 to 77.8% at age 21, before rising to 80% at ages 22 and 23. Table 4 shows that the highest percentage of symptoms in all three categories of ADHD is present among students aged 18 and 19, indicating that this age group may face more severe ADHD-related problems.
Table 5 shows the correlation between all related factors like age, gender, education level, parent education level, family type, siblings, and whether the student was staying in a hostel or their home was conducted, and ADHD symptoms responses and results show that there was no such correlation among them, so this all factors do not impact ADHD symptomatic higher educational students.
Fig. (1A) shows that the higher number of siblings had fewer symptoms. Fig. (1B) shows that the smaller the family, the higher the symptoms; similarly, Fig. (1C, D) show that the higher the parent's education level, the higher the symptomatic child till graduation, and in the master's level of education, the bar shows a lower number because a lower number of parents had done masters. Bartlett's Test of Sphericity, with a chi-square value of 1563.423 and 153 degrees of freedom, yields a p-value of 0.000, indicating significant correlations between variables. The Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO) value was 0.892, and Cronbach's alpha value was 0.859 for ADHD Self-Reported Symptomatic questionnaires (ASRS- v1.1). Table 6, which was made up of 18 questions, further confirms that the ASRS- v1.1 questionnaire was useful for checking adult ADHD symptoms in students of higher educational institutes.
Table 6 shows an 18-question mixture of 3 kinds of questions. 6 from each category: inattention (AT), hyperactivity (HA), and impulsivity (IM) symptoms scoring is shown in Table 1, which represents “sometimes” slightly higher scoring in the inattention category of symptoms.
| - | Age | Gender | No of Siblings | Family Type | Father E-L | Mother E-L | Hosteler/Day Scholar | |
|---|---|---|---|---|---|---|---|---|
| Inattention | Pearson Correlation | .001 | -.075 | -.049 | .002 | .025 | .014 | .062 |
| Sig. (2-tailed) | .986 | .156 | .349 | .973 | .631 | .786 | .244 | |
| Hyperactivity | Pearson Correlation | .020 | .004 | .003 | .043 | .009 | .016 | -.011 |
| Sig. (2-tailed) | .701 | .947 | .950 | .413 | .863 | .769 | .833 | |
| Impulsivity | Pearson Correlation | .000 | .084 | -.002 | .054 | -.021 | .009 | -.037 |
| Sig. (2-tailed) | .999 | .113 | .970 | .305 | .687 | .859 | .489 | |
| ADHD | Pearson Correlation | -.015 | .016 | -.055 | .019 | -.034 | -.003 | -.020 |
| Sig. (2-tailed) | .771 | .757 | .294 | .714 | .523 | .948 | .699 | |
| S.No | Questions | Never | Rarely | Some times | Often | Very Often |
|---|---|---|---|---|---|---|
| AT1 | How often do you have trouble wrapping up the final details of a project once the challenging parts have been done? | - | - | - | - | - |
| AT2 | How often do you have difficulty getting things in order when you have to do a task that requires organization? | - | - | - | - | - |
| AT3 | How often do you have problems remembering appointments or obligations? | - | - | - | - | - |
| AT4 | When you have a task that requires a lot of thought, how often do you avoid or delay getting started? | - | - | - | - | - |
| AT5 | How often do you fidget or squirm with your hands or feet when you have to sit down for a long time? | - | - | - | - | - |
| AT6 | How often do you feel overly active and compelled to do things, like you were driven by a motor? | - | - | - | - | - |
| HA1 | How often do you make careless mistakes when you have to work on a boring or difficult project? | - | - | - | - | - |
| HA2 | How often do you have difficulty keeping your attention when you are doing boring or repetitive work? | - | - | - | - | - |
| HA3 | How often do you have difficulty concentrating on what people say to you, even when they are speaking to you directly? | - | - | - | - | - |
| HA4 | How often do you misplace or have difficulty finding things at home or at work? | - | - | - | - | - |
| HA5 | How often are you distracted by activity or noise around you? | - | - | - | - | - |
| HA6 | How often do you leave your seat in meetings or other situations in which you are expected to remain seated? | - | - | - | - | - |
| IM1 | How often do you feel restless or fidgety? | - | - | - | - | - |
| IM2 | How often do you have difficulty unwinding and relaxing when you have time to yourself? | - | - | - | - | - |
| IM3 | How often do you find yourself talking too much when you are in social situations? | - | - | - | - | - |
| IM4 | When you’re in a conversation, how often do you find yourself finishing the sentences of the people you are talking to before they can finish them themselves? | - | - | - | - | - |
| IM5 | How often do you have difficulty waiting your turn in situations when turn-taking is required? | - | - | - | - | - |
| IM6 | How often do you interrupt others when they are busy? | - | - | - | - | - |
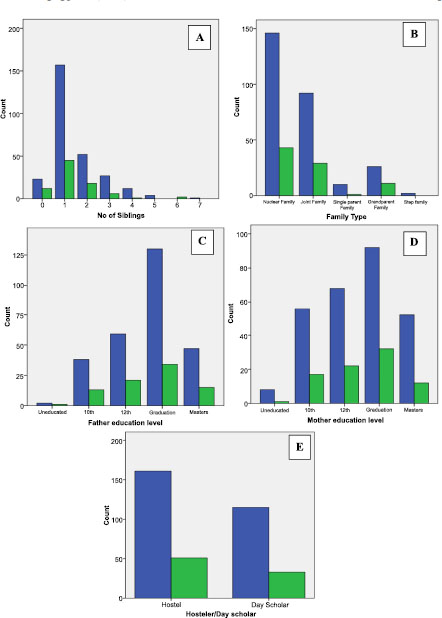
This figure shows the number of symptomatic (green bar) and non-symptomatic (blue bar) students as per their A-Number of siblings, B-Type of Family, C-Father Education Level, D-Mother Education Level, and E- Student staying in the hostel had the more symptom of ADHD compared to students traveling their educational institute from the home or staying out of campus.
4. DISCUSSION
The present study included ages 17 to 23 years, both male and female students from higher educational institutes pursuing their undergraduate courses. This study used Self-Report Scales for ADHD (ASRS-v1.1) questionnaires that contain 18 questions. The ASRS-v1.1 questionnaires indicate that most students reported experiencing ADHD symptoms 'sometimes.' This suggests that ADHD-related issues are present in higher educational institutions, affecting areas such as education, sports, and social interactions.This study found that the prevalence of ADHD symptomatic students was 23.3%, where inattention was 35%, hyperactivity was 39.2%, and impulsivity was 26.9%. An analogous study was carried out in Pakistan in 2018 by Nida Tabassum Khan, who studied undergraduate students at BUITEMS to determine the prevalence of adult Attention Deficit Hyperactivity Disorder (ADHD). The results showed that 36% of the students had ADHD [24]. In Karnataka, India, Bhushan Shashi did a 2018 study on a group of 20 + 1.45 years old. Researchers discovered that the prevalence of ADHD among university-level health science students was 20.20% [25]. In 2019, Meng Shi conducted a study in China to investigate the relationship between personality traits and internet addiction in Chinese medical students. The study also looked at the mediating role of symptoms of attention-deficit/hyperactivity disorder. The results showed that the prevalence of inattention among medical students was 44.7%, with 35.5, 8.6, and 0.6% of students presenting mild, moderate, and severe symptoms of ADHD in the 17 to 26-year-old age group [33]. Researchers also discovered that people with internet addiction were more likely than those without it to experience indications of ADHD [34]. Internet addiction among students was not examined in the current study. In 2019, Takashi Ohnishi conducted a study in Japan with the goal of determining the prevalence and patterns of psychiatric comorbidities in adult attention-deficit/hyperactivity disorder in a routine clinical setting and the study's mean age was 33.07 SD 9.79 years, and the findings showed that 336 (58.43%) of the patients were inattentive, 40 (6.96%) were hyperactive-impulsive, and 301 (52.35%) were patients with comorbidities [35]. In order to determine how informative self-reported adult ADHD symptoms were, Michael J. Silverstein conducted a study in 2018 in New York City, the study titled “An Examination of the Agreement Between the Adult Attention-Deficit/Hyperactivity Disorder Self-Report Scale V1.1 and Adult Attention-Deficit/Hyperactivity Disorder Investigator Symptom Rating Scale” revealed that inattention was more common than hyperactivity, with the combination of both being 36.8% and hyperactivity being 1.2%. The combination of both, with ADHD along with a few other factors, made up 2.9%, and the mean age group was 28.8 SD 8.6 years [30]. Michael J. Silverstein's 2019 study in Philadelphia, USA, was carried out in continuation with the goal of validating the expanded versions of the Adult ADHD Investigator Symptom Rating Scale and the Adult ADHD Self-Report Scale v1.1 Symptom Checklist. Here, they consider the age group 32 SD 10.5 years, and they also find out the prevalence of ADHD was 57.20% [31]. The current study was conducted by Pearson correlation to establish the correlation between age, gender, education, number of siblings, family type, education of mother and father, and hostel or day scholar with ADHD symptoms, but did not find any relation among them. Each question response data shows that as the age increases, the symptoms decrease, and female students show higher symptoms compared to male students. This may be because more female students have participated in this study. One of the studies conducted by Thakur in 2019 found that visual attention was similar in students with and without hearing impairments. The only difference observed was in divided attention, which was better in students with hearing impairments [36].The study conducted by Roberta Waite [32] in 2020 at Wynnewood, USA, assessed ADHD symptoms among university students using the ASRS v1.1 Examining associations with social anxiety and self-efficacy in individuals aged 19 to 20 years, a study found a prevalence of ADHD at 10.80%. Another study conducted by Michael J. Silverstein in 2018 in Boston, USA, assessed the test-retest reliability of the Adult ADHD Self-Report Scale (ASRS) v1.1 Screener in non-ADHD controls from a primary care physician practice, with participants averaging 38.1 years of age (SD = 10.8). This study found a prevalence of ADHD at 11.25% [29], which was lower compared to the current study.There was another observational study conducted in Ahmedabad, India, in 2021 to find out the prevalence of attention deficit hyperactivity disorder - ADHD among Young Individuals aged between 18 and 24 years. They found that the overall prevalence was 11.40%, where Inattentive was 5.53%, and Hyperactive/Impulsive was 6.64% [34]. Michael Rösler conducted a literature review on attention deficit hyperactivity disorder (ADHD) in adults in 2010 and found that the overall prevalence of ADHD was 4.40% [37, 38], where most of the studies conducted by using adult ADHD Self-Report Scale (ASRS) v1.1 were found to be higher, and the study conducted by assessment of ADHD as per proper diagnostics guideline was found to be less, this is because the questionnaires mainly assessing the symptoms of ADHD, which can verry as per students education levels like graduation, post-graduation, and ethnicity and race, most of the study conducted in Asian continent found to had more prevalent compared the other western countries. Many alternative therapies, aside from medical treatments, exist for managing ADHD and its symptoms [39-41]. These therapies, which have been used for treatment purposes, need further exploration to enhance attention levels in students with ADHD and support their academic, sports, and social lives [42, 43].
CONCLUSION
The present study found that the adult ADHD Self-Report Scale (ASRS) v1.1 questionnaires were a well-established tool for checking ADHD symptoms among the adult population. The prevalence rate of ADHD symptoms among higher educational institutes was 23.3%, and individual symptoms of inattention (35%), hyperactivity (39.2%), and impulsivity (26.9%) were present among ADHD-symptomatic students. This study also finds out that age, gender, education level, parent education level, family type, number of siblings, and whether the student is staying in a hostel or their home do not impact ADHD symptoms among university students in Punjab, India. This study found that the prevalence rate of ADHD symptoms was high among university students, and this can affect education, concentration, and other learning and sports-related activities among students. Students should focus on reliving such symptoms and improving their daily activity outcomes. This study also suggests further ADHD clinical diagnosis. Students with ADHD should go for vision therapy and psychological, neurological, and occupational therapy for better outcomes and performance. Also, a vision therapy framework needs to be established to find out which kind of vision therapy is more reliable and repeatable for improving ADHD symptoms.
LIMITATION
This study was conducted only on university students, and ADHD Self-Report Scale (ASRS) v1.1 questionnaire was utilized to find out the prevalence of ADHD instead of clinical diagnosis and psychological diagnostics.
AUTHORS’ CONTRIBUTION
R.T: Study conception and design; S.S: Data collection; K.K: Data analysis and interpretation of results; A.D.: Formatting and Helping in writing;
B.R.T: Contributed to the study’s concept and design; S.S: Collected the data; K.K: Interpreted the results and analyzed the data; A.D: Contributed to the formatting and writing of the study.
LIST OF ABBREVIATIONS
| ADHD | = Attention-Deficit/Hyperactivity Disorder |
| EEG | = Electroencephalography |
| NLP | = Natural Language Processing |
| CNN | = Convolutional Neural Networks |
| MRI | = Magnetic Resonance Imaging |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Punjab Ethical Committee at Chitkara University, Punjab, India, for conducting this study. An ethical clearance certificate was obtained with ethical registration no. IHEC/CU/PB/DHR/23/182.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.


