All published articles of this journal are available on ScienceDirect.
Arachnoiditis Ossificans – A Rare Cause of Progressive Myelopathy
Abstract
Arachnoiditis ossificans is a rare cause of chronic, progressive myelopathy. In contrast to the more common benign causes of meningeal calcification, arachnoiditis ossificans results in replacement of portions of the spinal arachnoid by bone as an end-stage complication of adhesive arachnoiditis. It is usually the sequela of prior trauma or interventional procedures. Prognosis and treatment options depend upon the location and degree of spinal stenosis with thoracic involvement being more common and more severe than lumbar spine involvement. The imaging findings on magnetic resonance imaging may be confusing; however, the findings of intraspinal ossification on computed tomography are characteristics and diagnostic. We present a classic case of arachnoiditis ossificans in an elderly man who presented with progressive myelopathy and a recent fall, along with a review of the literature. The imaging in this case not only identified the characteristic findings of arachnoiditis ossificans but also identified secondary findings of the underlying causative etiology.
INTRODUCTION
Arachnoiditis ossificans is a rare entity characterized by ossification within the arachnoid as a result of end-stage adhesive arachnoiditis. Patients often suffer from progressive, debilitating neurological deficits. Most reported cases have an underlying history of trauma or interventional procedures, to include spinal surgery. Arachnoiditis ossificans is clinically and radiographically distinct from the far more common benign etiologies of meningeal calcification, as are seen with age-related degeneration and abnormalities in calcium metabolism. We present a case of arachnoiditis in an 89-year-old man who presented with long-standing myelopathy and a history of a recent fall, as well as a comprehensive literature review.
CASE PRESENTATION
An 89-year-old man with a long-standing history of progressive myelopathy presented to the emergency room for evaluation after a fall from standing. The patient stated that he felt weak in his bilateral lower extremities prior to his legs “giving out” and falling. He denied loss of consciousness or significant localizing pain.
On presentation, the patient was cognitively intact, aside from some memory impairment. Neurologically, the patient had bilateral motor weakness of the lower extremities with relatively normal sensation and reflexes.
Past medical history revealed prior lower back trauma with a resultant disc herniation, which required surgical intervention decades earlier. This history was elicited from the family after imaging evaluation, since the patient was a relatively poor historian. The patient had limited medical follow-up but reported progressive, worsening lower extremity weakness, which was more pronounced over the past year. Ultimately, the patient required the use of a walker to assist with ambulation as a result of his myelopathy.
The patient underwent magnetic resonance imaging (MRI) of the lumbar spine, which demonstrated a focal region of increased T2 signal intensity with volume loss involving the lower thoracic cord, consistent with myelomalacia from prior cord injury (Fig. 1). Findings of arachnoiditis were noted, including peripheral displacement and regions of central clumping of descending nerve roots of the cauda equina (Fig. 2). Decreased T2 signal intensity was visualized along the dura, dependent portions of the distal thecal sac, along the descending nerve roots of the cauda equina, and within the central portion of the distal thecal sac with corresponding regions of intermediate and hypointense signal intensity on T1 sequences (Fig. 3). The MRI appearance suggested calcification/ossification and/or hemosiderin from prior trauma. Computed tomography (CT) was subsequently performed, demonstrating mineralization along the dura and ossification within the central thecal sac, compatible with arachnoiditis ossificans (Fig. 4).

Axial (A) and sagittal (B) T2-weighted image through the distal thoracic cord demonstrate increased cord signal intensity with cord volume loss, consistent with myelomalacia (arrows).
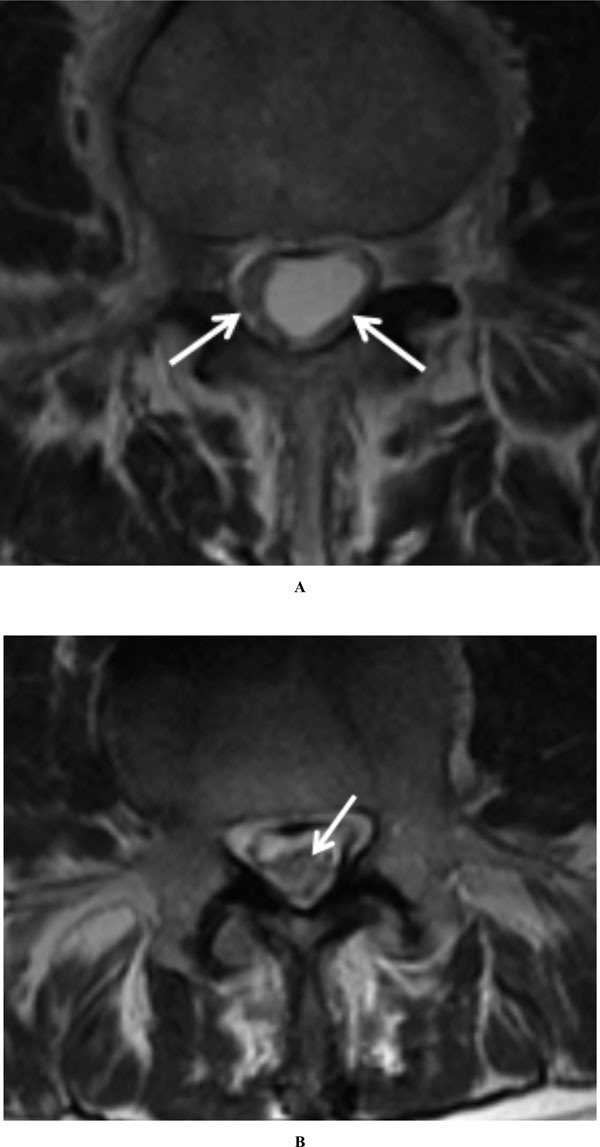
Axial T2-weighted images demonstrate peripheral (A, arrows) and central (B, arrow) displacement of the descending nerve roots of the cauda equina, consistent with sequelae of arachnoiditis.
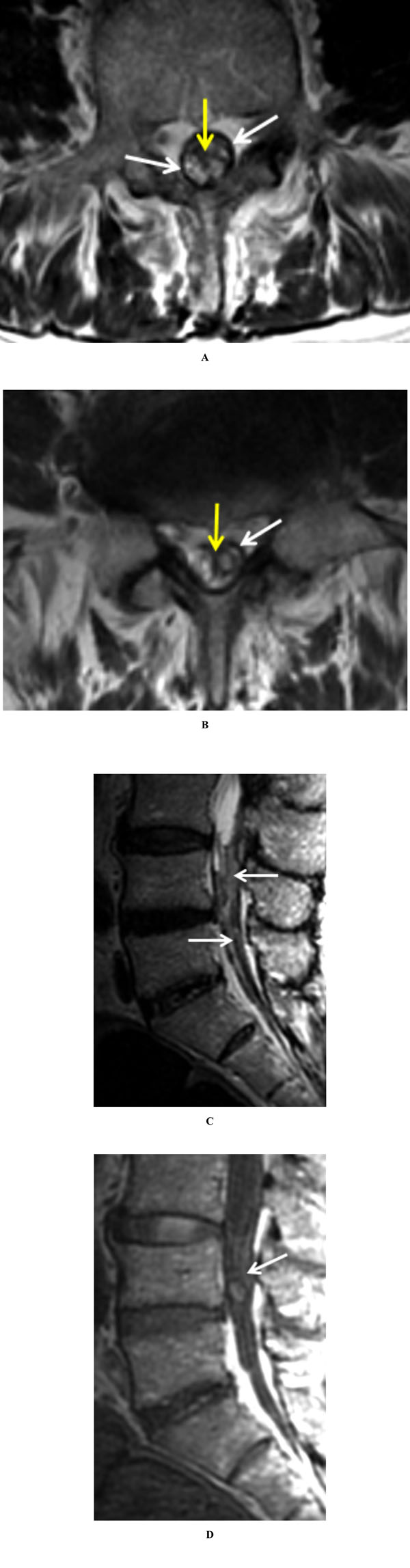
Axial T2-weighted images (A and B) reveal abnormal thickening and decreased signal intensity along the dura (white arrows), as well as central decreased signal intensity within the thecal sac and along the descending nerve roots of the cauda equina (yellow arrows). Sagittal T2-weighted image (C) demonstrates the intrathecal hypointense signal abnormality at the L4 and L5 levels (arrows), which is intermediate to hypointense on sagittal T1-weighted image (D, arrow).
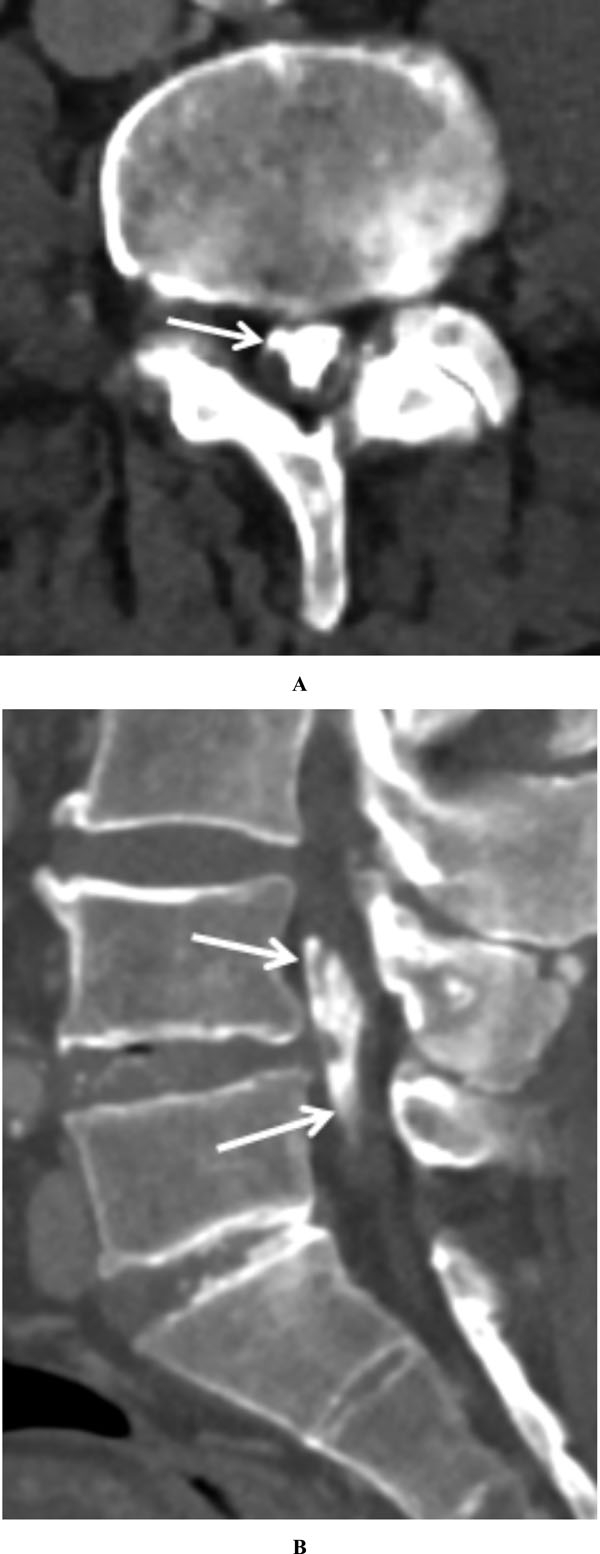
Axial CT image through the lower lumbar spine (A) demonstrates central ossification with the thecal sac (arrow), corresponding to regions of T2 hypointensity on MRI (Fig. 3A). Sagittal reformatted image (B) demonstrates the craniocaudal extent of the arachnoid ossification (arrows). Multilevel degenerative changes are partially visualized.
Due to the patient’s underlying clinical status and primary involvement of the lumbar spine, the decision was made to treat the patient’s progressive myelopathy conservatively rather than surgically.
DISCUSSION
Spinal arachnoiditis ossificans is a rare disease with fewer than 80 cases reported to date [1, 2]. This entity, characterized by pathologic ossification of the arachnoid, is thought to represent the sequelae of end-stage adhesive arachnoiditis. It is important to distinguish this potentially debilitating disease from other entities that result in benign meningeal calcification (rather than ossification), as they will have different implications for imaging evaluation and treatment strategies. These forms of meningeal calcification within the spine are not uncommon with incidences being reported as high 76% in autopsy studies [3]. Common causes include age-related degenerative mineralization, renal failure, hyperparathyroidism, and other hypercalcemic states. This is in contradistinction to arachnoiditis ossificans, which appropriately describes replacement of portions of the spinal arachnoid by bone and has not been shown to have an association with calcium metabolism [4].
Histologically, arachnoiditis ossificans is characterized by osteoblasts with clusters of arachnoidal cells. It is believed that mature bone arises from these arachnoidal cells that have the capability of multipotent differentiation [5]. This osseous metaplasia can occur secondary to any process that incites chronic inflammation, such as prior hemorrhage, infection, surgery, or myelography. The majority of reported cases include a history of either trauma or iatrogenic injury [1]. Most cases occur in the thoracic spine, which correlates to the region of highest concentration of arachnoidal cells, followed by the lumbar spine [6]. Patients typically present with chronic back pain and neurological deficits, such as lower limb weakness. Symptoms are generally more severe when ossifications are located within the thoracic spine, presumably due to the less ample space within the central canal relative to the lumbar spine and associated cord compression.
Given the presenting symptoms, it is not unusual for MRI to be the first imaging modality utilized. Imaging features typically include findings of arachnoiditis with irregular thickening and clumping of nerve roots of the cauda equina. The regions of arachnoid ossification can have a similar appearance to calcification on MRI, ranging from hypointense to intermediate in signal intensity on T1 and T2 sequences, as well as hemosiderin when hypointense. While the diagnosis may not be as clear on an MRI, it is essential to document the extent of neural involvement and to identify potential coexisting pathology such as syringomyelia or intrathecal cysts [7, 8]. Occasionally, secondary imaging findings may be identified to suggest an underlying etiology, as was the case with our patient. Unenhanced CT better demonstrates the presence and extent of arachnoid ossifications and is thus complementary to MRI. This ossification of the meninges should be readily distinguished from benign meningeal calcifications on CT, which can be seen in a number of settings, to include age-related degeneration, renal failure, hyperparathyroidism, or other hypercalcemic states, as well as calcification of the ligamentum flavum. Unlike arachnoiditis ossificans, these benign calcifications would not primarily involve central intrathecal structures.
The rarity of this diagnosis makes a standard treatment option difficult to establish. Clinical outcomes with conservative and surgical treatment options have been mixed, and are thus decided on a case-by-case basis. Domenicucci et al. formulated a classification pattern based on the radiological features in order to assess treatment options and compared clinical outcomes [9]. Type I is described as a semicircular pattern that involves a portion of the thecal sac; Type II is described as a circular pattern that involves the circumference of the thecal sac; and Type III is characterized as ossification that affects the entire contents of the thecal sac at the involved level [9]. In terms of localization, Type I was found primarily in the thoracic spine, Type III exclusively in the lumbar spine, and Type II in either the thoracic or lumber spine with thoracic being more common. Based upon this system, Type I and II patterns were more likely to proceed for surgery, which generally consisted of decompressive laminectomy, while Type III cases were managed medically. Approximately half of those treated surgically showed improvement while those with isolated lumbar ossifications showed satisfactory results with medical management, although they did not usually present with severe neurological symptoms initially compared to patients with thoracic involvement [9].
CONCLUSION
Arachnoiditis ossificans is a rare entity characterized by ossification within the arachnoid as a result of end-stage adhesive arachnoiditis. In contrast to patients with benign meningeal calcifications, patients with arachnoiditis ossificans often present with progressive, debilitating neurological deficits. On CT, the imaging findings are characteristic and diagnostic, demonstrating ossification within the spinal canal. The MRI findings, however, are less specific and may be confused with regions of calcification or hemosiderin. Occasionally, secondary imaging findings may be identified to suggest an underlying etiology, as was the case with our patient. It is therefore important for radiologists to be aware of and consider this rare entity when faced with a case of apparent arachnoiditis on MRI that demonstrates atypical signal intensity within the spinal canal.
CONFLICT OF INTEREST
The views expressed in this material are those of the authors and do not reflect the official policy or position of the U.S. Government, Department of Defense, or United States Air Force.
ACKNOWLEDGEMENTS
Declared none.


