All published articles of this journal are available on ScienceDirect.
A Thyroglossal Duct Cyst Carcinoma Mimics Ranula: A Case Report and Literature Review
Abstract
Background
A thyroglossal duct cyst (TGDC) is a common congenital anomaly. However, the development of carcinoma within it is rare. Submental presentation and the concomitant TGDC carcinoma with thyroid gland carcinoma are indeed very rare.
Case Presentation
In this case report, a TGDC carcinoma with concomitant thyroid carcinoma in a fifty year-old Iraqi middle aged female presented with a submental mass. It was diagnosed initially as a sublingual ranula. Clinical examination showed a non-mobile tender hard mass at the submental region with no obvious thyroid gland enlargement. An imaging study showed a normal thyroid size and texture with a complex cystic-solid lesion involving the sublingual space. Fine needle aspiration cytology showed atypical follicular epithelial inflammatory cells within the thyroid nodule.
Conclusion
The neck mass smear suggested papillary thyroid carcinoma, which was confirmed on surgery by Sistrunk procedure and postoperative histopathology. Subsequently, the patient was kept on radioactive iodine therapy. Papillary thyroid carcinoma arising in TGDC may present as a large complex midline mass at the upper neck or floor of the mouth and should be kept in mind even if there is no history of thyroglossal duct cyst or a history of thyroid nodule.
1. INTRODUCTION
The thyroglossal tract is an embryonic remnant that originates during embryonic life when the thyroid gland descends from the foramen cecum to its location in the anterior neck. This remnant could be presented as a tract, cyst, duct, or fistula [1]. If this remnant fails to be involuted, thyroglossal duct cysts (TGDC) may develop, which is the most common congenital cervical anomaly; its prevalence is about 7% in the general population [2]. One of the complications of TGDC is the development of carcinoma; approximately 1% of thyroid carcinoma develops in the TGDC and the median age of diagnosis is the 4th decade of life [3]. Carcinoma of thyroglossal duct cyst is a well-known entity, being more common in females and 40-year-olds. Most carcinomas are small (up to 1.5 cm) and do not extend beyond the cyst. As with the thyroid gland, papillary carcinoma is the most common type. Concomitant carcinoma arising in TGDC and the thyroid gland is extremely rare [4], and in the majority of cases, thyroid carcinoma is only diagnosed post-operatively.
The presentation of TGDC in most of the previously reported cases has been reported to be a midline neck mass. However, a TGDC in an aberrant location, like lateralized neck mass [5] or submental mass [6], is possible and makes the diagnosis more challenging. Adding to this is the fact that patients are often asymptomatic. The differential for cystic mass in the floor of the mouth includes ranula, dermoid cyst, and thyroglossal duct cyst. Although previous reports indicate most cystic lesions on the floor of the mouth, when evaluated by imaging, to result in a ranula as the diagnosis [7], differentiation between the three conditions is critical as their clinical implication and management completely differ [7]. Diagnosis requires imaging techniques, like ultrasound, with the excisional biopsy being the gold standard for the diagnosis [8-10]. With limited facilities and the absence of local guidelines in low-income countries, this aberrant presentation represents a diagnostic challenge. The diagnosis of TGDC carcinoma is critical to ensure timely and appropriate treatment. Comprehensive clinical evaluation, imaging studies, and cytological examination are essential to avoid misdiagnosis. Healthcare providers should maintain a high index of suspicion for malignancy in atypical cystic neck masses to mitigate adverse outcomes.
We herein report a case of a thyroglossal duct cyst harboring papillary carcinoma and microcarcinoma within the thyroid gland in an Iraqi middle-aged female patient that presented as a submental mass and was diagnosed initially as a ranula.
2. CASE PRESENTATION
A 50-year-old Iraqi female patient presented to the outpatient clinic at al-Yarmouk Teaching Hospital Baghdad, Iraq, with a complaint of painful swelling on the floor of the mouth for one year that increased in size over the last month; the swelling was not associated with difficulty in swallowing or hoarseness of voice and there was no recent history of febrile illness and no family history of thyroid malignancy. The clinical examination showed a hard, non-mobile tender mass about 1 cm in size at the midline of the submental region with a focal bulge at the floor of the mouth with no erythema or other signs of inflammation and it did not transilluminate; thus, the surgeon suggested ranula as the initial diagnosis.
The thyroid gland was not palpable upon physical examination; hormonal assessment showed normal thyroid function tests as follows: T3 = 2.1 (reference range: 0.92-2.79 ng/dl), T4 = 7 (5-12 mcg/dl), TSH = 3 (0.5-4.1mU/L). The ultrasound of the neck (Fig. 1) revealed the thyroid lobes to be normal-sized and of normal echogenicity, having a heterogeneous texture with multiple variable sizes and echogenicity nodules; some showed a spongiform appearance, some were echogenic, and others were hypoechoic. The largest nodule was hypoechoic sub-centimetric on the Lt lobe, measuring 9x7 mm, with a well-defined complex, cystic, and solid mass at the submental region. The solid component of the mass was highly vascular lying to the Lt side, showing tiny non-shadowing echogenic foci (microcalcification) (Fig. 1B). As for the cystic component of the mass, it had a thin wall and it lay on the Rt side of the mass. A few enlarged lymph nodes adjacent to the mass showed cortical thickening, and the largest one measured 20x10 mm.
A non-contrast CT scan (Fig. 2) showed a normal thyroid gland in size and texture. The complex cystic-solid lesion involving the sublingual space measured 25x30x51 mm = 18 cc volume, having microcalcifications within the solid component and the wall of the cystic component.
The solid component measured 20x18 mm. The cystic component insinuated at the floor of the mouth between the right genioglossus, right hyoglossus, and right mylohyoid muscles abutting the central part of the hyoid bone.
Fine needle aspiration (FNA) cytology was performed on the left thyroid nodule and the suprahyoid mass under ultrasound guidance, and it showed atypical follicular epithelial inflammatory cells within the thyroid nodule. The smear from the neck mass also showed an atypical epithelial cyst arranged in three-dimensional aggregates featuring a high N/C ratio, suggesting papillary thyroid carcinoma.
Following multidisciplinary team consultation, surgery was performed by an experienced surgeon on the patient in the form of total thyroidectomy, central neck dissection with complete excision of the mass with safe margin (using the Sistrunk procedure), lymph node (LN) clearance of levels 1, 2, and 6 LN group, and excision of the body of the hyoid bone (Fig. 3). The surgeon noticed that the mass reached the floor of the mouth just below the oral mucosa. The surgery was uneventful, and the patient was discharged home without any post-operative complications. The case was referred to the oncologists for many sessions of radioactive iodine therapy.
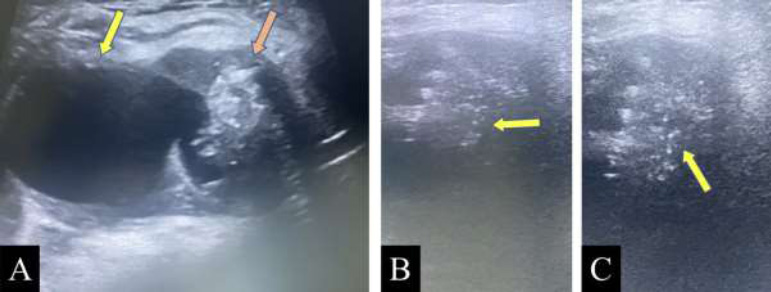
Ultrasound image of the submental region using a linear probe. A: Complex mass containing cystic component (yellow arrow) and solid component (orange arrow). B and C: Microcalcification within the solid components (yellow arrow).
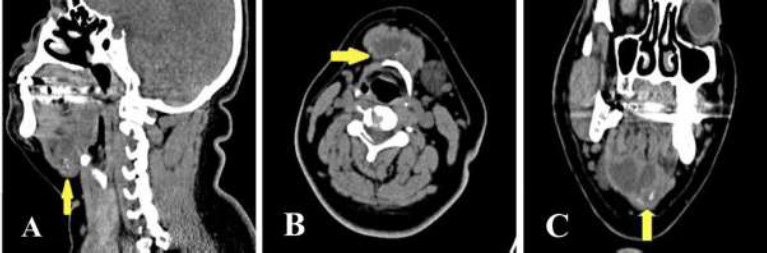
Non-contrast CT scan of the neck. A: Sagittal reformatted section. B: Axial section. C. Coronal section showing the complex mass at the submental region abutting the central part of the hyoid bone (yellow arrow) with foci of microcalcification within the solid component (blue arrow).
Histopathological examination of the submental mass showed the solid component consistent with papillary thyroid carcinoma invading the connective tissue and vascular structure. The cystic component was consistent with the thyroglossal duct cyst. Sections from the thyroid tissue showed a small part of encapsulated papillary thyroid carcinoma measuring 2 mm (Fig. 4). Eight regional lymph nodes were tumor-free (pathological stage T4aN0).
3. DISCUSSION
TGDC is a common congenital midline neck swelling in infants and children [11], although it is not uncommon in adults. A recent case series of collected TGDCs over nine years reported a bimodal age distribution. The first peak was observed at a mean age of 6 years, while the second peak was observed at a mean age of 42 years [11, 12]. The reported case in the current study was of a fifty year-old female, who was older than the age range of 20 to 31 years described in the literature [12]. Nevertheless, the patient contemplated seeking medical assistance at this age, rather than the precise age of presentation. She recalled experiencing pain and swelling a year before, despite the fact that the mass may have been present prior to this time without any specific complaint.
TGDCs can develop anywhere along the line from the foramen caecum to the anatomical position of the thyroid gland [13]; however, 60% are observed at hyoid and infrahyoid levels [10] and are usually diagnosed clinically. Midline and suprahyoid lesions usually require supporting imaging and diagnosing cytology [11]. Intralingual thyroglossal duct cysts are exceedingly uncommon, constituting only 2% of all reported cases. They are particularly challenging to identify and are treated differently when they manifest in the sublingual region. Functional impairments, including dyspnea, dysphagia, dysphonia, and difficulty digesting, are associated with TGDCs that develop in this region or an oral floor [13]. Apart from swelling at the base of the mouth and mild pain, our patient did not complain of any of these functional impairments. The differential diagnosis of TGDCs at this site may include ranula, cystic hygromas, dermoid cysts, or epidermoid cysts [14].
The clinical examination of our case revealed a hard, immobile tender mass at the midline of the submental region with a focal bulge at the floor of the mouth mimicking a ranula. Ultrasound examination depicted a highly vascularized solid and cystic mass at the submental region with occasional microcalcification and adjacent suspicious lymph nodes. The lesion's extent was further determined by a non-contrasting CT scan, which depicted lesion borders between the right genioglossus, right hyoglossus, and right mylohyoid muscles confronting the central part of the hyoid bone. In addition to accurately delineating the anatomy of the lesion, preoperative CT was essential for the differentiation of thyroglossal duct cysts from other lesions, the identification of functioning thyroid tissue in the neck, and highlighting the possible malignant change within the cyst [15-18]
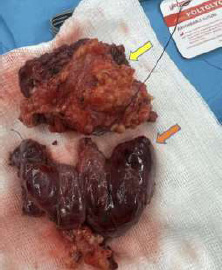
The gross surgical specimen of total thyroidectomy (orange arrow) with an excision of the submental mass (yellow arrow).
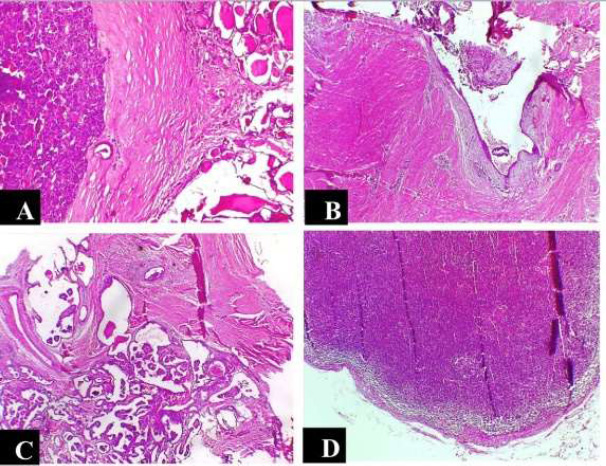
The pathological specimen.A: Solid nodule of thyroid carcinoma with thick capsule. (H&E, 4X). B: Thyroglossal cyst lined by squamous epithelium (H&E, 4X). C: Papillary thyroid carcinoma within thyroglossal cyst infiltrating the adjacent skeletal muscle (H&E, 4X). D: The cervical lymph node showing no metastatic disease (H&E, 4X).
| - | Authors/Refs. | Year | Age | Gender | Presentation | Method of Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Kojima [22] | 1996 | 34 | Female | Submental swelling | CT | Sistrunk procedure |
| 2 | Asakage [23] | 1997 | 47 | Female | Submental swelling for 13 years | FNA | Sistrunk procedure |
| 3 | Naghavi [24] | 2003 | 28 | Male | Paramedian mental swelling | CT | Sistrunk procedure |
| 4 | Arabi [25] | 2007 | 41 | Male | Growing submental mass over a few months with dysphagia and hoarseness | Histopathology | Sistrunk procedure |
| 5 | Mesolella et al. [26] | 2010 | 27 | Male | Painless swelling in the submental region, gradually enlarging over 3 months and extending to the tongue | CT with contrast | Sistrunk procedure |
| 6 | Albayrak [27] | 2011 | 39 | Male | Throat swelling | Histopathology | Sistrunk procedure |
| 7 | Yamada [28] | 2013 | 74 | Female | Lateral submental swelling | CT | Sistrunk procedure |
| 8 | Seow-En et al. [29] | 2015 | 15 | Male | Painless submental neck mass gradually enlarging over 2 years | Core needle biopsy under GA | Sistrunk procedure |
| 9 | Feng [30] | 2015 | - | Female | Asymptomatic submental mass for 2 months | CT | Sistrunk procedure |
| 10 | Cheon [31] | 2016 | 17 | Female | Asymptomatic submental mass for 2 months | CT | Sistrunk procedure |
| 11 | Van Beck et al. [32] | 2019 | 20 | Female | Painless submental neck mass enlarging and becoming painful postpartum with painful swallowing | Fine-needle aspiration | Sistrunk procedure |
| 12 | Gómez-Álvarez [33] | 2022 | 30 | Female | Progressive swelling for 1 year | US, CT | Sistrunk procedure |
| 13 | Koda et al. [34] | 2023 | 80 | Female | Painless swelling for 10 years | CT and FNA | Sistrunk procedure |
| 14 | Pazmino [35] | 2023 | Old age | Female | Dysphagia for 2 years | US and FNA | Sistrunk procedure |
| 15 | Murgod [36] | 2024 | 30 | Female | Painless swelling | CT and FNA | Sistrunk procedure |
The development of thyroglossal duct cyst carcinoma can be attributed to either the spread of cancer from a thyroid gland tumor or to carcinoma originating in the thyroglossal remnant. The reported cases have endorsed both hypotheses since synchronous thyroid carcinoma (supporting metastasis hypothesis) has been confirmed in only one-third of the cases [15].
As a result of the rarity of the condition, studies addressing the epidemiology and risk factors of malignant transformation in TGDC are contradicting. While earlier studies have described the malignant transformation in children and adolescents [19, 20], Rayess and colleagues have found in a systematic review of ninety-eight relevant articles that malignant transformation presents at a mean age of 39.5 years (9-83 years) with female predominance [21]. Over the last twenty-five years, fifteen cases of sublingual TGDC carcinoma have been documented (Table 1), all of which have included primary papillary thyroid carcinoma. In keeping with our findings, the majority of the reported cases have shared the same history, characterized by the absence of primary thyroid disease, an asymptomatic enlarging submental mass, and normal thyroid function tests. The age range of these cases has been 15-80 years with a male-to-female ratio of 1:3.
Carcinoma was diagnosed in our 50 year-old patient by FNA with features of papillary thyroid carcinoma. Radiologically, her thyroid gland was of average size, showing multiple tiny nodules with various echogenicity, none of which were suspicious. In agreement with similar studies, the Sistrunk procedure was performed with total thyroidectomy, and no postoperative complications were reported.
The standard Sistrunk procedure involves en bloc resection of the body of hyoid bone with the cyst and suprahyoid musculature by midline neck incision and it represents the gold standard surgical procedure for TGDC since the newer procedures, including the modified Sistrunk procedure, have been found to have comparable results and complications to the standard procedure [37]. A robot-assisted surgery involving the retroauricular incision was tried, which exhibited unclear advantages other than aesthetics by avoiding the neck scar [38].
Surgery for TGDC cancer is a controversial topic. While some surgeons maintain that the Sistrunk technique is adequate for patients who do not show symptoms of disease spread, new evidence suggests that a complete thyroidectomy should also be done [39]. The majority of low-risk patients undergo Sistrunk treatment, which entails opening the oral cavity at the foramen cecum after removing the cyst from the thyroglossal duct using the middle portion of the hyoid bone and a core of tissue surrounding the thyroglossal tract [40]. It is commonly linked to complete thyroidectomy in patients at high risk [41-44]
Thyroidectomy also allows for the continuation of optional radioactive iodine treatment and improved utilization of thyroglobulin levels for monitoring and follow-up [33].
The American Thyroid Association (ATA) in 2019 stated the use of radioactive iodine as an adjuvant therapy in differentiated thyroid carcinoma aimed at post-operative remnant ablation to reduce the chance of recurrence and enhance the treatment of metastatic disease and recurrent disease in tumors with proven avidity [45-48].
Multiple limitations can be noted in the reporting of this case, such as a lack of long term follow-up data to evaluate the outcomes and recurrence rates following the chosen surgical approach and the decision to perform a total thyroidectomy alongside the Sistrunk procedure being primarily based on emerging evidence and similar studies rather than direct case specific findings of disease spread, which limit the generalizability of the findings [49]. In addition, the absence of molecular or histopathological details, such as BRAF or other genetic markers commonly associated with papillary thyroid carcinoma, also restricted the depth of the diagnostic and prognostic analysis [50].
CONCLUSION
In this case, a thyroglossal duct cyst presented as a submental mass that progressively increased in size, harboring a thyroid papillary carcinoma. The possibility of TGDC carcinoma should be kept in mind when facing such a presentation even if there is no history of thyroglossal duct cyst or thyroid nodule, regardless of the age and gender of the patients.
AUTHORS’ CONTRIBUTION
M.N.H.M.D.: Study concept and design: WNMH; methodology; Y.A.A.A.L.A.: Analysis and interpretation of results; N.N.A.: Visualization; S.K.A., Q.A.H.: Drafting of the manuscript. All authors have reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| TGDC | = Thyroglossal duct cyst |
| FNA | = Fine needle aspiration |
| LN | = Lymph node |
| ATA | = American Thyroid Association |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the ethics committee of the Al-Kindy College of Medicine in Baghdad, Iraq (204; 4/5/2023).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient and the patient was informed that all the findings and outcomes might be used for scientific publication, depending on their relevance.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
ACKNOWLEDGEMENTS
Declared none.


