Features of Neurotoxicity on Brain CT of Acutely Intoxicated Unconscious Patients
Abstract
Diagnostic imaging is a valuable device in clinical management of poisoned patients presenting to emergency units in a comatose state. Some toxic agents have adverse effects on the central nervous system (CNS). Non-contrast computed tomography (CT) of the brain, as an available diagnostic method with a high resolution, can provide useful information about structural disturbances of unconscious patients with suspected drug or chemical intoxication. The authors would describe various presentations of toxic substances detected on the brain CT scans of ten patients with acute intoxication. While non-specific, CT findings of low-attenuation lesions in the basal ganglia, infarctions in young patients, or diffuse edema should raise suspicion for poisoning or overdose.
INTRODUCTION
Poisoning refers to the development of dose-related adverse effects following exposure to chemicals, drugs or other xenobiotics [1]. Poisoning is the third cause of injury-related mortality, with a frequency of 11%, in the United States [2].
Poisoned patients present to medical centers in a number of ways. Some are known to be victims of a toxin. For these patients, diagnostic radiology can be a valuable tool in assessing adverse impacts of toxin on the patient. Other patients present in comatose state or with symptoms not recognized clearly as being related to a toxic substance. In such cases, physicians should always consider the possibility of any association between a clinical or radiologic finding with an unrecognized toxin [3].
The development of cranial computed tomography (CT) and its widespread use in clinical practice has facilitated the recognition of toxin-associated brain abnormalities. The clinical value and diagnostic accuracy of brain CT scan, has been emphasized in former reports. Several toxic brain lesions such as cerebral atrophy, intracranial hemorrhage, cerebral edema, ischemia and infarction have all been reported on brain CT scans obtained from patients who intoxicated by various toxic agents. For example, cerebral edema and severe depression have been noted after intoxication with carbon monoxide [4], methanol [5], propranolol [6], etc. Focal ischemia and infarction, especially in the region of globus palidus, has been described following cocaine (3, 4-methylenedioxymetamphetamine) abuse [7, 8]. Brain disturbances frequently have been reported after accidental or suicidal consumption of methanol consisted of bilateral putaminal necrosis, diffuse white matter necrosis, cerebellar and hypothalamic focal lesions [9].
Toxicologic causes of intraparenchyma and subarachnoid hemorrhage include cocaine or other sympathomimetic drugs, and also methanol intoxication [7, 10, and 11].
Basal ganglia and white matter changes occur following poisoning due to carbon monoxide, methanol, ethylene glycol, cyanide, hydrogen sulfide, mercury, manganese, heroine, barbiturates, and solvents [12, 13].
In patients with loss of consciousness due to poisoning, associated brain injury should be evaluated. For this reason, correct application of neuroimaging techniques, and particularly brain CT scan as an available device, would be helpful in appropriate management of patients. These images provide emergency medical staff with a wide range of brain findings in different anatomic regions, most frequently in the basal ganglia.
Here, we introduce brain CT findings of 10 patients who presented to our university hospital after acute exposure to different toxic substances.
MATERIALS AND METHODOLOGY
This cross-sectional study was performed in Loghman-Hakim Poison Hospital in Tehran, Iran between March and August 2006. This hospital is the biggest tertiary referral center in Iran and usually 28,000 emergency ward presentations due to poisoning are registered annually [14]. Ten interesting patients following exposure to toxic agents who were unconscious upon presentation were selected to report in this article. The patients were in comatose state, and none of them had any documented CNS structural disorders earlier. The accurate diagnosis of those who lost their life during hospitalization was confirmed by postmortem examinations.
Imaging Protocol
CT scans were performed during the first three to four hours of hospitalization with one scanner (Shimadzu, 7800, Japan) using the sequential techniques (collimation 10 mm, spacing 10 mm). CT window widths ranged from 100 to 120 Hounsfield Unit (HU) and levels ranged from 35 to 49. In the presence of head trauma, bone window was performed with window widths 2000 and level 400, then radiological features were determined .No oral or intravenous contrast medium was applied for the images.
RESULTS
Case 1
A 20-year-old male was brought to the emergency unit in comatose state after methamphetamine (crystal) abuse. Before presentation, he experienced three episodes of seizure, perspiration, palpitation and altered behaviors. At admission, physical examination showed systolic blood pressure (BP) of 60 mmHg; pulse rate (PR) of 120 per minute, and his respiratory rate (RR) was 30 per minute. Laboratory findings revealed a metabolic acidosis. On the brain CT scan, extensive temporo- parieto-occipital infarction in left cerebral hemisphere was observed (Figs. 1a-1c).

Extensive temporo-parieto-occipital infarction in left cerebral hemisphere in methamphetamine (crystal) intoxication.
Case 2
A 19-year-old man with no significant past medical history was presented in a comatose state nearly two hours after ingestion of 1200 mg of propranolol in a suicidal attempt. He experienced cardiac arrest in another hospital, for which successful cardiopulmonary resuscitation (CPR) was performed, before referral to our center. At admission, vital signs showed a systolic BP of 50 mmHg, and a RR of 30/minute, with a filiform pulse. Pupils were symmetric without any reaction to light. He underwent brain CT scan which revealed bilateral basal ganglia hypodensities and cytotoxic edema with pseudo-subarachnoid hemorrhage sign (Figs. 2a-2c). After eight days of receiving supportive treatments, the patient died due to cardiac arrest.
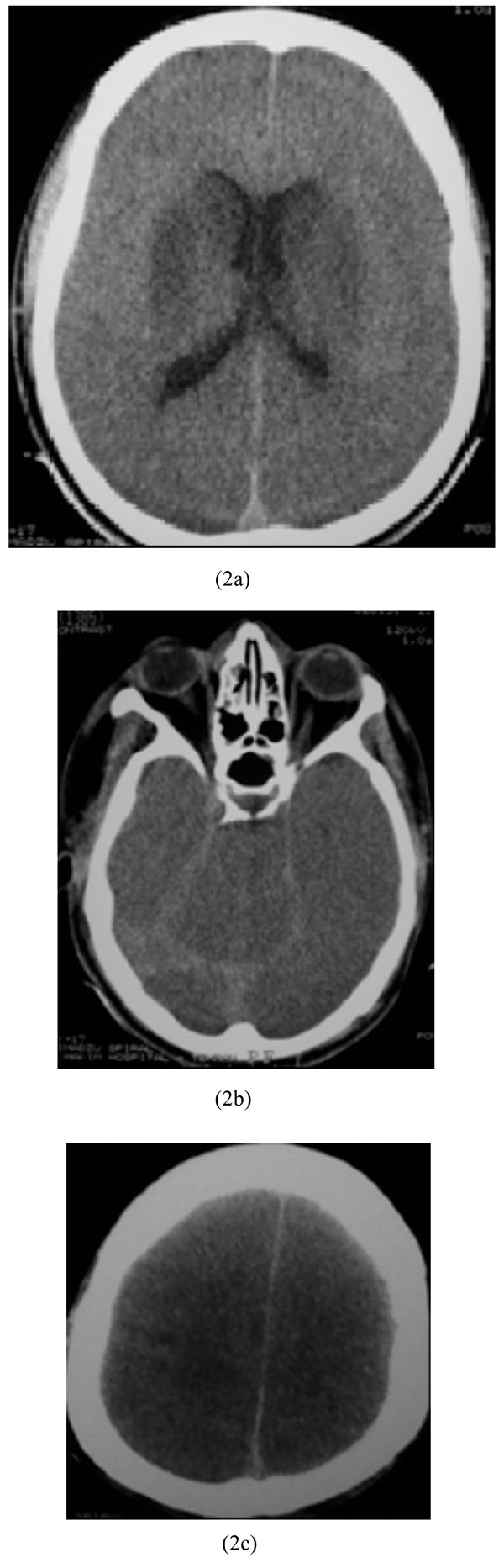
Bilateral basal ganglia hypodensities and cytotoxic edema with pseudo-subarachnoid hemorrhage sign in propranolol intoxication.
Case 3
A 42-year-old man was admitted due to carbon monoxide (CO) poisoning. On physical examination, he was comatose with no other considerable finding. Laboratory data revealed acidosis with no abnormal glucose or electrolyte level. Brain CT scan without contrast medium showed bilateral hypodensity of glubus pallidus nucleuses (Fig. 3).

Bilateral hypodensity of glubus pallidus nucleuses in carbon monoxide (CO) poisoning.
Case 4
A 54-year-old man was brought to our hospital three hours after ingestion of 900 mg of chlordiazepoxide in a suicide attempt. Lab data’s revealed: acidosis with no abnormal glucose or electrolytes level. Brain CT scan showed diffuse massive supratentorial cytotoxic edema with sparing of infratentorial region (Figs. 4a-4c).
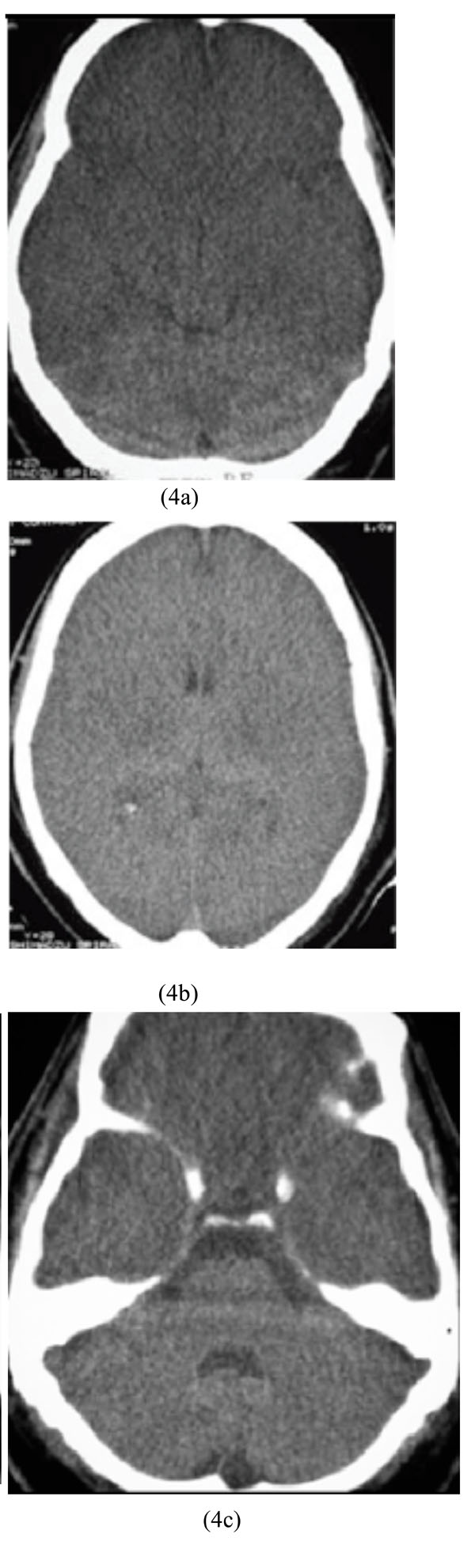
Diffuse massive supratentorial cytotoxic edema with sparing of infratentorial region in chlordiazepoxide overdose.
Case 5
A 19-year-old man was referred to our hospital 30 hours after accidental methanol ingestion instead of ethanol. He was comatose but his family said he had reported blurred vision before becoming unconscious. Laboratory data showed severe metabolic acidosis and normal blood sugar. Ophthalmologic examination revealed papillary edema and optic disc hyperemia. Brain CT scan study before hemodialysis demonstrated bilateral basal ganglia and external capsule hypodensities with hemorrhagic focus in left side. Parasagital hypodensity was also observed (Figs. 5a-5c).
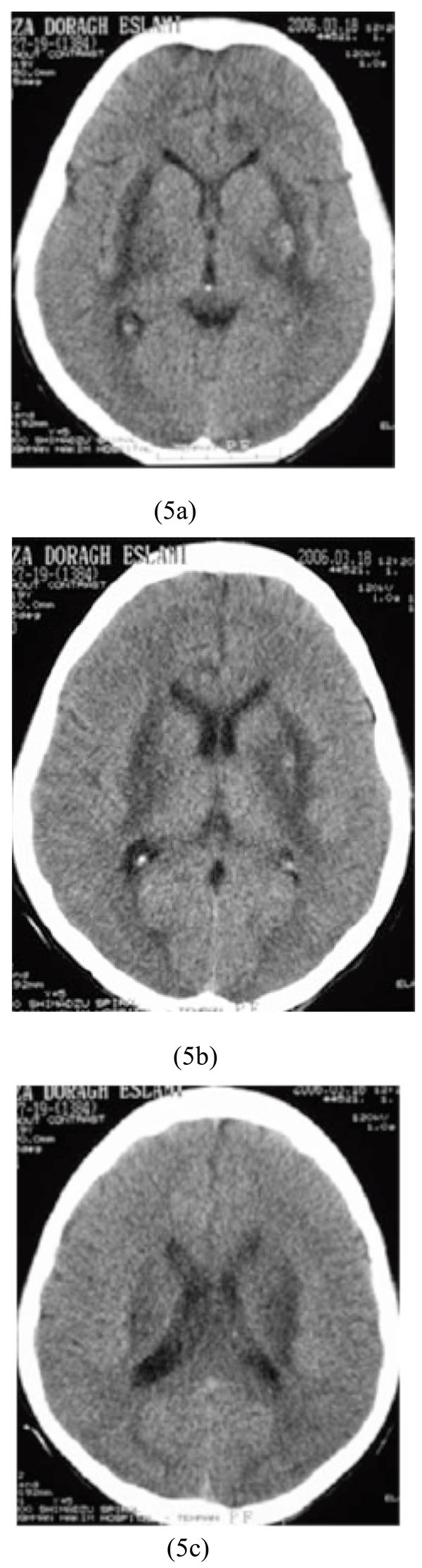
Bilateral basal ganglia and external capsule hypodensities with hemorrhagic focus in the left side along with parasagital hypodensity after accidental methanol ingestion.
Case 6
A 27-year-old woman, previously diagnosed by major depression, who decided to commit a suicide, was brought to our hospital three hours after ingestion of 750 mg of amitriptyline. On physical examination, her BP was 150/90 mmHg, PR of 110/min, and RR of 12/min. Laboratory data revealed a metabolic acidosis with no abnormal blood glucose or electrolyte levels. Electrocardiogram revealed tachyarrhythmia. Brain CT scan showed diffuse supratentorial cytotoxic edema with sparing of infratentorial region (Figs. 6a-6c).

Diffuse supratentorial cytotoxic edema with sparing of infratentorial region associated with amitriptyline poisoning.
Case 7
A 26-year-old crack (purer form of heroin) abuser man was admitted to our hospital. Physical examination showed: BP=110/70, PR=90/min, and RR=16/min. Brain CT scan showed massive supratentorial cytotoxic edema and pseudosubarachnoid hemorrhage sign as obviously reversed gray and white matter differentiation with sparing of infratentorial region. Also, a focus of hypodensity involving the left basal ganglia was observed (Figs. 7a-7c).
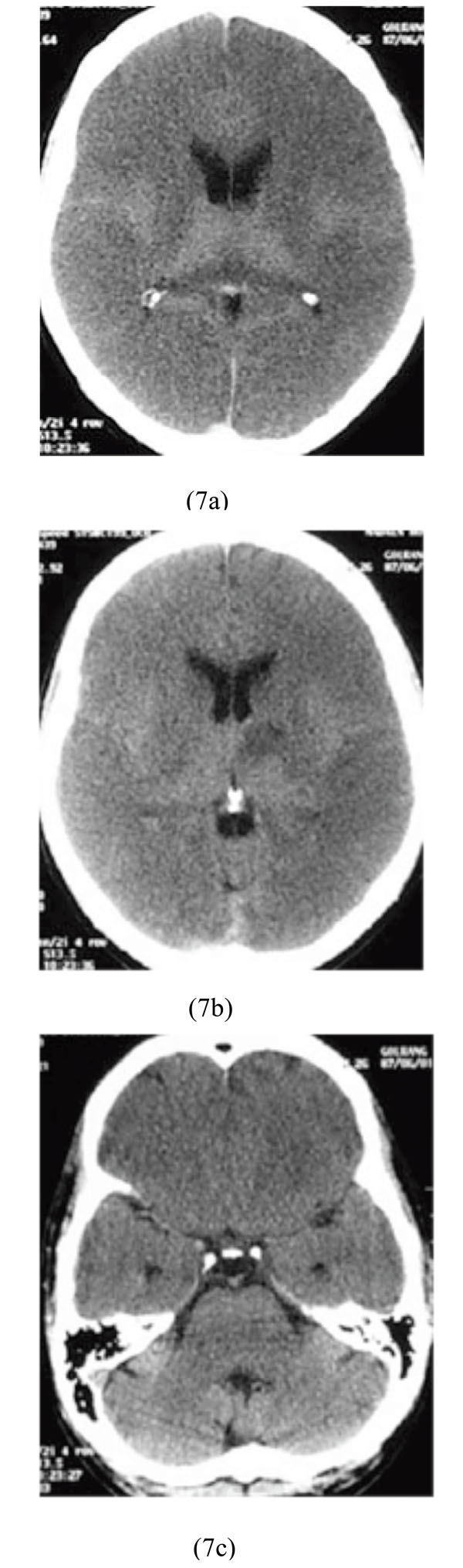
Massive supratentorial cytotoxic edema and pseudosubarachnoid hemorrhage sign with sparing of infratentorial region along with left basal ganglia. hypodensity after poisoning with crack (heroin).
Case 8
A 21-year-old male farmer was admitted because of suicidal ingestion of organophosphate toxin. His symptoms started with sweating, headache, nausea and vomiting, muscular weakness, and dizziness. Upon admission, he had pin-point pupils which followed by loss of consciousness, urinary incontinence and finally seizure. His vital signs were as follows: BP=90/60, PR=50/min, RR=12/min. Brain CT scan showed bilateral hypodensity lesions of the basal ganglia indicative of infarctions (Figs. 8a-8b).
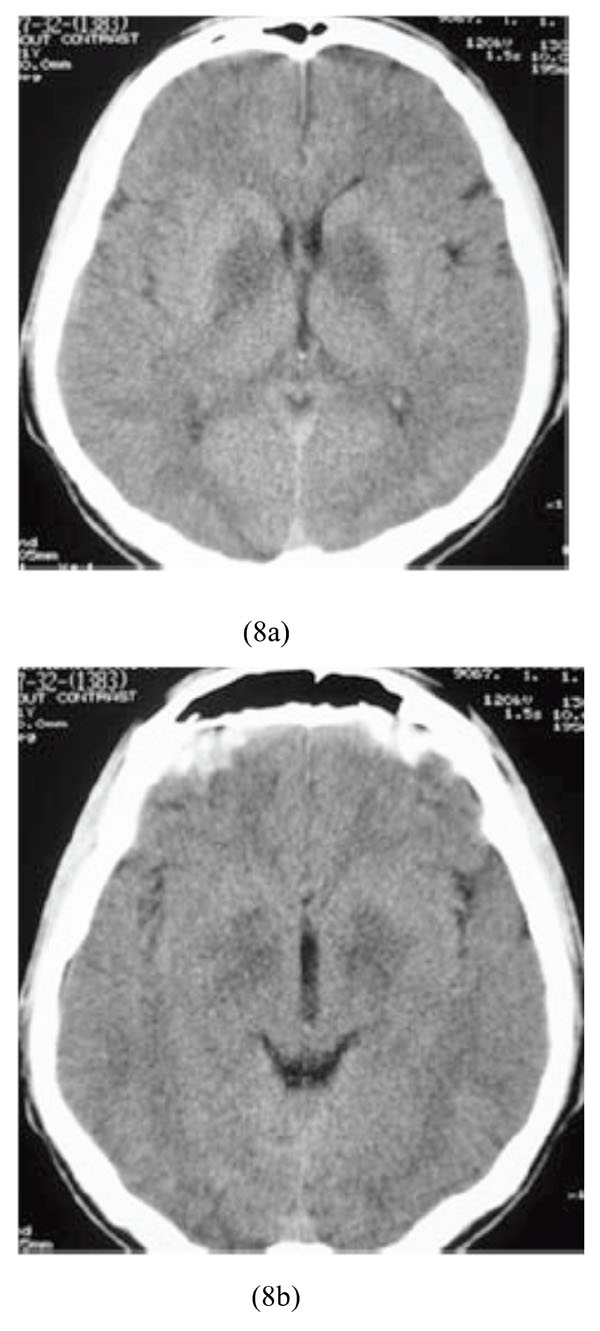
Bilateral hypodensity lesions of the basal ganglia indicative of infarctions following ingestion of organophosphate toxin.
Case 9
A 32-year-old heroin abuser man was hospitalized due to non-cardiogenic pulmonary edema and right hemiparesia as a result of heroin intoxication. Physical examination showed: BP=90/60, PR=90/min, RR=12/min and right hemiparesia. He underwent brain CT scan which revealed left frontal lobe infarction (Figs. 9a-9b).
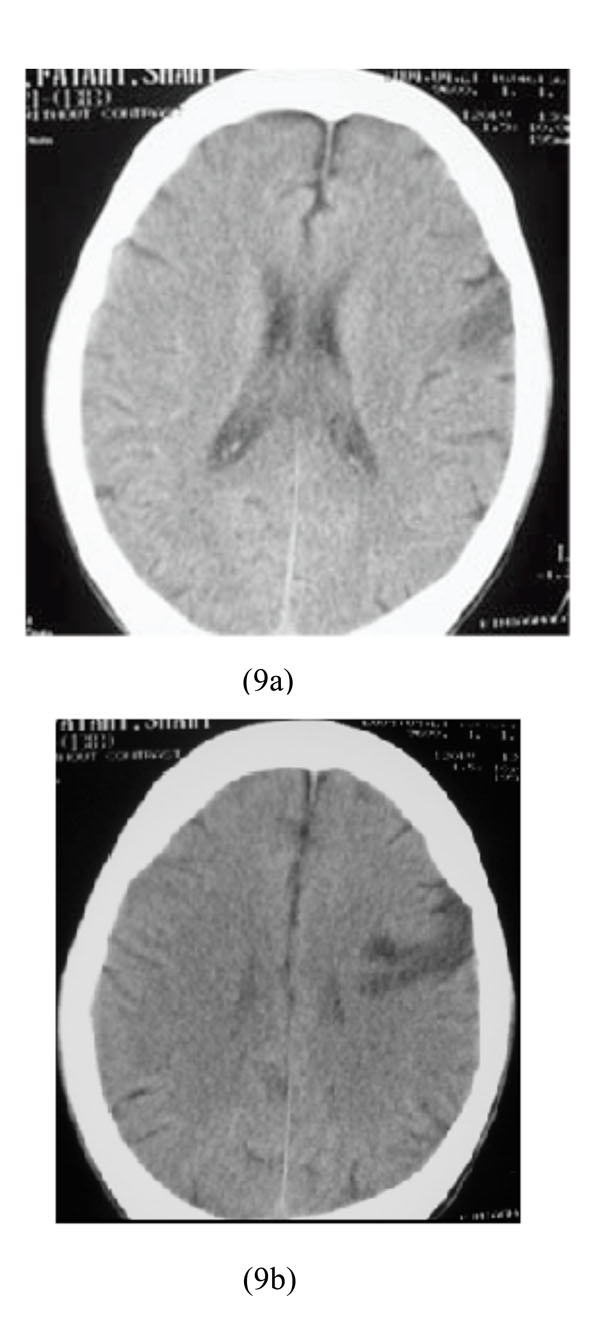
Left frontal lobe infarction in heroin intoxication.
Case 10
A 20-year-old man, who decided to commit a suicide with insulin injection, was brought to our hospital in comatose state with a blood sugar level of 15 mg/dL. He was admitted and then treatment with intravenous glucose was initiated. Brain CT scan showed diffuse bilateral supratentorial cytotoxic edema and pseudo-subarachnoid hemorrhage sign (Figs. 10a-10c).
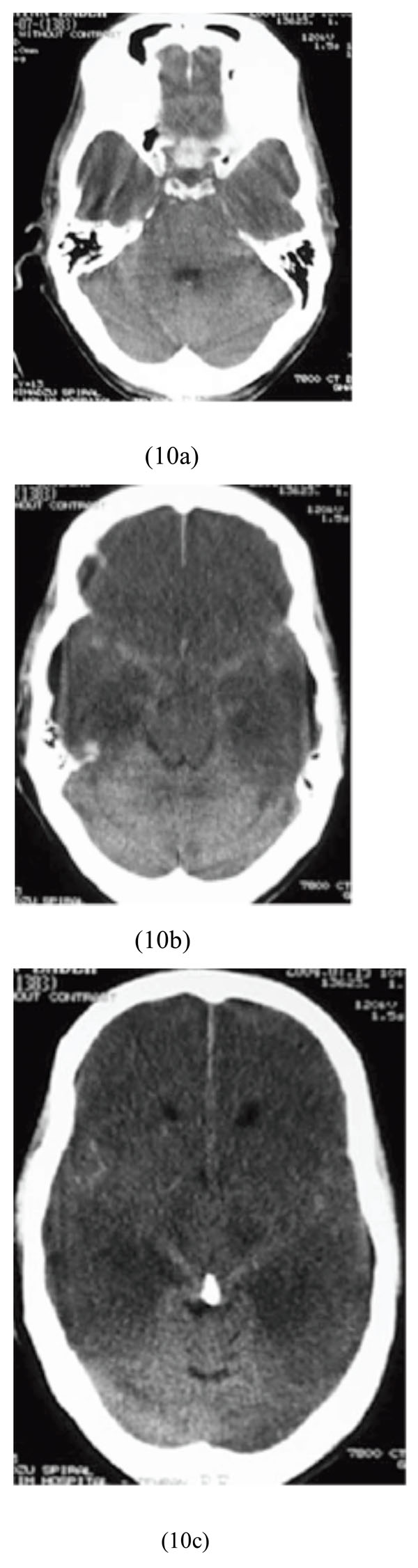
Diffuse bilateral supratentorial cytotoxic edema and pseudosubarachnoid hemorrhage sign after insulin injection and severe hypoglycemia.
DISCUSSION
Non-contrast computed tomography (CT) of the brain, as a worthwhile radiological method, can guide the emergency staff to make a more accurate diagnosis and better medical management of unconscious patients with suspected drug or chemical intoxications. Cytotoxic edema and hpodensity lesions of the basal ganglia were the most common findings in this population. In our center, specific laboratory methods to detect various chemicals or drugs abused are not always available. Therefore, reported signs on brain CT scans presented in this article may increase the awareness of emergency radiologists, and also clinical toxicologists with respect to various neuroimaging findings of drugs and chemicals.
CONCLUSION
While non-specific, CT findings of low-attenuation lesions in the basal ganglia, infarctions in young patients, or diffuse edema should raise suspicion for poisoning or overdose.


